For any questions about prior authorization please call Customer Service at the number on the back of your Blue Shield. Menu under Blue Cross Blue Shield of Michigan.
Https Www Ibx Com Documents 35221 56677 Prior Auth Botulinum Toxins Pdf 99b5b638 Fc7c 290b Ab03 58c7a997ef40 T 1580924446000
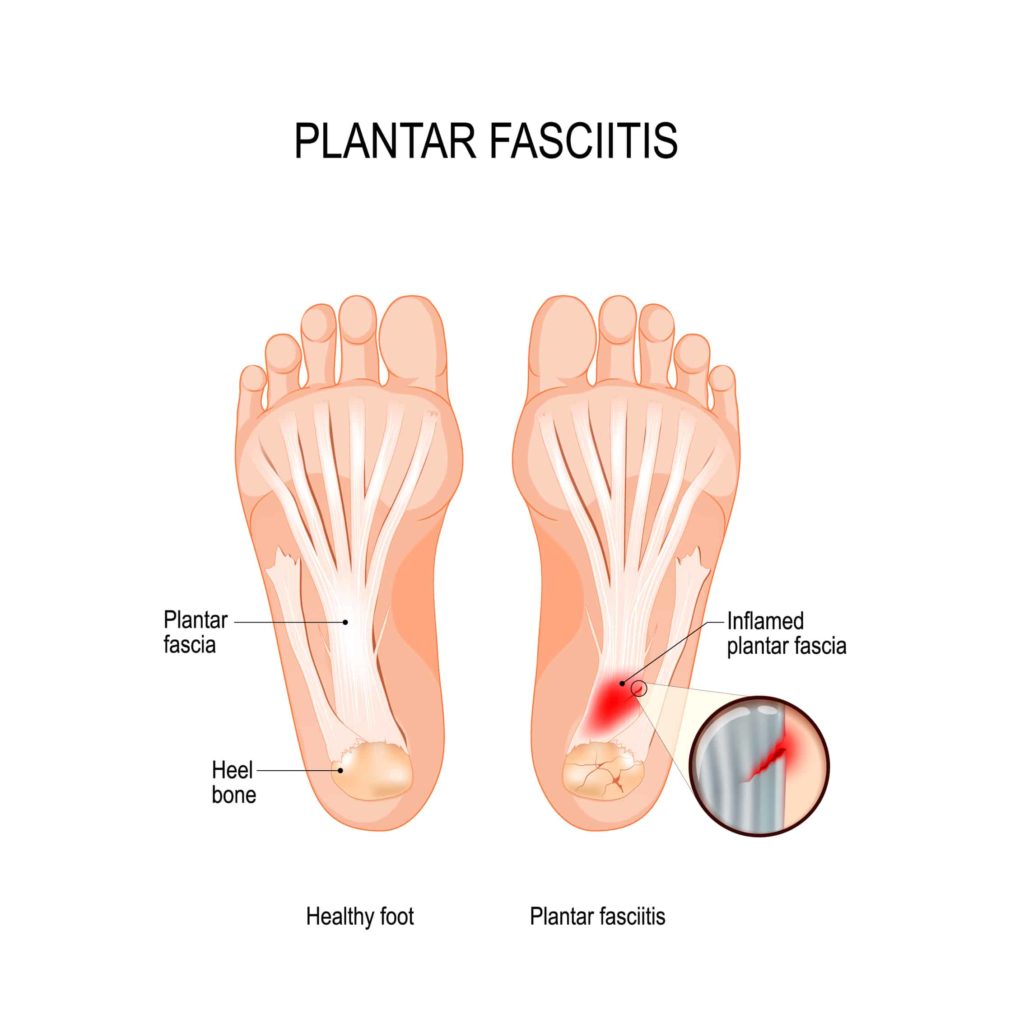
Chronic migraine is defined as episodes that otherwise meet criteria for migraine eg at least 4 hours in duration that occur on at least 15 days per month for more than 3 months in the absence of medication overuse.
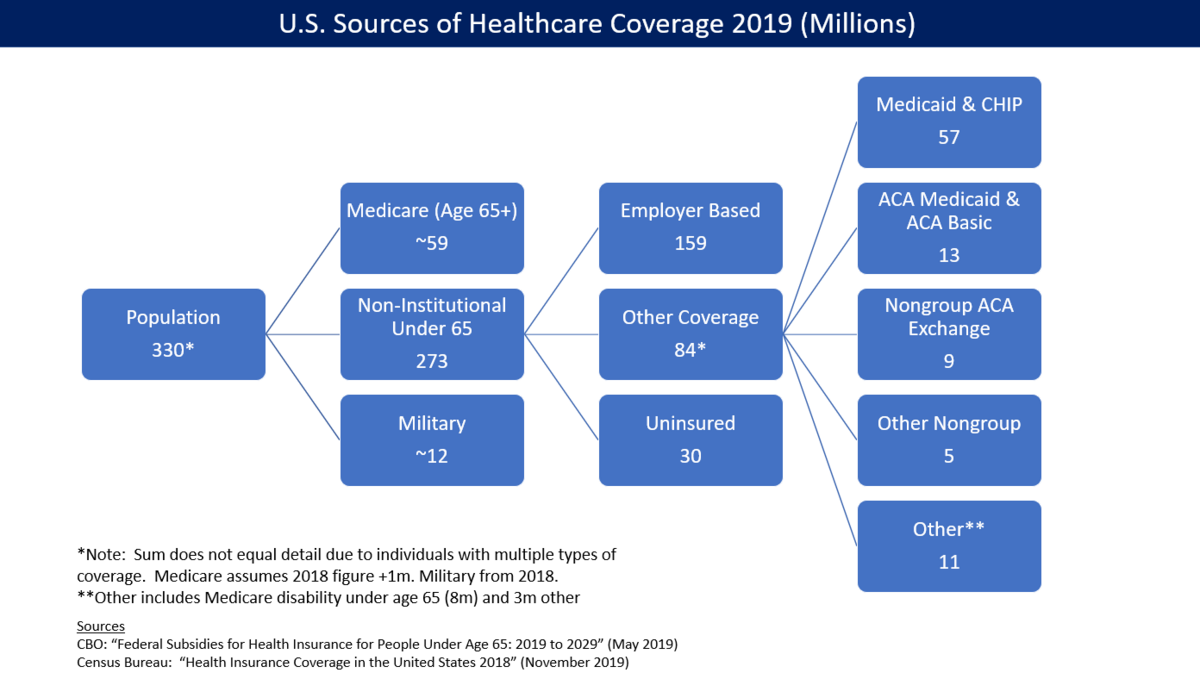
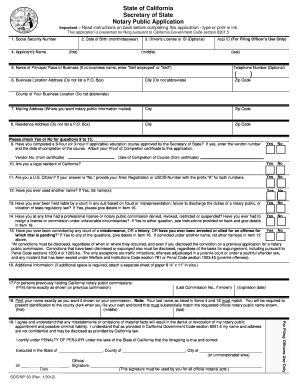
Does blue cross blue shield cover botox for migraines. Depending on your health insurer you may be able to your out of pocket expense. Prior Authorization Program. If your entry is on the list then you will need to work with your doctor to get prior authorization before Blue Shield will pay.
Dru006 is available for Botox Type-A injection. Just enter the procedure or drug name in the Search for Procedures field. For patients with functional impairment due to spasticity or for conditions of involuntary muscle contraction due to several conditions if it is.
For drugs covered under the commercial Blue Cross or BCN pharmacy benefit please see. You would have to reach out to your insurance company to see what their policy is. Migraine headache duration reduced at least 100 hours per month.
Find out how our medication policy which determines if a service will be covered by a plan is reviewed and updated. Alberta Blue Cross plan members who currently have Botox or Xeomin prescribed for a condition can obtain their prescription with no change in process until July 31 2015. You can find out more about that here.
Added requirement for trial and failure of cGRP prior to approval for Botox. I would also recommend a consultation with a provider in your area so you are able to discuss. US based Allergen offer funding program you can find out more about if your insurer does not cover Botox for migraine or if you dont have insurance.
Remember its always important to check that the service or drug you need is a covered benefit under your plan. Botox which is made from the toxin of certain bacteria is much more expensive than other migraine treatments like beta blockers which are available as generics. Medical decisions relative to medical technologies are to be made strictly by memberspatients in consultation with their health care providers.
They have been putting a lot of efforts to improve quality of health care and coverage. Continuation of therapy requires documented positive clinical response. Bluecross Blueshield Association is a health insurance provider which has been in existence for more than 75 years.
Added step through Dysport AND Xeomin prior to Botox. Since its FDA approval in 1991 Botox has been used for a wide variety of off-label indications. Blue Cross Blue Shield No Blue Cross Blue Shield considers nerve decompression surgery experimental and investigational.
Follow-up treatment may be claimed in 12 week intervals. Division of Health Care Service Corporation a Mutual Legal Reserve Company an Independent Licensee of the Blue Cross and Blue Shield Association Page 3 of 3 Section IV RimabotulinumtoxinB Myobloc Diagnosis. This list applies to all BCN commercial members with medical coverage and Blue Cross commercial members that are subject to the PA program.
Access the Electronic Provider Access EPA via local Blues Plan Download the Registration form for electronic access from the Medical Prior Authorization Review link AND Submit the Registration form. This program ensures the medication is medically necessary and appropriate for your situation. For a single Botox visit you can expect the cost to be around 700 before any rebates.
Botox costs about 4800 a year. However effective August 1. JANUARY 2020 BLUE CROSS AND BLUE SHIELD OF ALABAMA 3 Botox Medical PA REVISED Effective 1120 For migraines.
For Cervical Dystonia. Members will receive a letter from Blue Cross. For chronic migraine the frequency or duration for chronic migraines will be reduced from the time of initial presentation with treatment by at least.
Generally all contracts need approval for Botox Type-A prior to coverage. A recent review of botulinum toxin for episodic migraines. APRIL 2021 BLE CROSS AND BLE SIELD O ALABAMA 1 Drug Guide and Clinical Program Updates Prime Therapeutics Pharmacy and Therapeutics PT Committee in association with Blue Cross and Blue Shield of Alabamas Formulary Business Committee recently approved updates to the Drug Guides and made clinical program changes to select medications.
Preauthorization is required for BlueCHiP for Medicare members and recommended for all other BCBSRI products for the Botulinium Toxin A or B for the treatment of migraines or hyperhidrosis. Botox and Xeomin coverage will only be approved if it is being used for its Health Canada-approved uses not if used for cosmetic purposes. All these indications are associated with dystonia ranging from achalasia spasticity after strokes cerebral palsy and anal fissures.
Type B currently has FDA approval for cervical dystonia and Botox onabotulinumtoxinA for the prevention of chronic migraine. Out-of-State Providers In order to be able to submit your prior authorization requests electronically you will need to. Botox treatment may be used for chronic migraine sufferers for persons aged 18 to 65 who suffer from migraines more than 15 times a month and have been recommended for this treatment by their physician.
We have a lot of patients who benefit from Botox in terms of reducing their migraines however. Centene Corp No Information Available NA Cigna No Information Available NA Health Net Varies by case Medical necessity criteria for the review of occipital nerve stimulation ONS also called peripheral nerve stimulation PFS a form of. Botox for migraines may be covered by your insurance though this varies greatly per plan.
In addition to broadening indications Botox has also been used in children under 12 for the treatment of cerebral. FDA approved dosing e. Drugs costs for affected benefit plans.
Only one call may be claimed regardless of the number of injections performed. The Blue Cross and Blue Shield Association does not intend by the FEP Medical Policy Manual or by any particular medical policy to recommend advocate encourage or discourage any particular medical technologies.