Key features of this option include. Print and save a PDF of the response.
 Tricare4u Authorization Fill Online Printable Fillable Blank Pdffiller
Tricare4u Authorization Fill Online Printable Fillable Blank Pdffiller
First you will need to go to your regional contractors website.
Tricare prior authorization online. Download and print the form for your drug. In the Secure Portal click on Submit Authorization Request to access CareAffiliate. Use our step-by-step WARF Guide and Request Type Guide.
Be sure an authorization is in place so you dont have to pay for the services out of pocket. You dont need to take action. Non-network providers are encouraged to submit online as electronic requests save time and improve accuracy.
Ordering care providers will complete the notificationprior authorization process online or over the phone. TRICARE covers medically necessary and appropriate testing. Getting prior authorization means youre getting the care approved by your regional contractor before you actually go to an appointment and get the care.
You do not need an approval from HNFS for medically necessary testing. You can view or check the status of your Tricare prior authorization form online through the Tricare website. The Prior Authorization Referral and Benefit Tool allows you to easily determine if an approval from Health Net Federal Services LLC HNFS is required.
Network providers requesting prior authorization for an elective admission or submitting an inpatient admission notification are required to submit online. Humana Military Health Net Federal Services and International SOS Assistance extended some already-approved referrals and authorizations that expired between March 1 2020 and June 30 2020. Use our step-by-step CareAffiliate Guide as a resource.
Prior authorization requests should be submitted at least 14 calendar days prior to the date of service or facility admission. This tool allows you to easily determine HNFS approval requirements. This automatic extension is for an extra 180 days from the expiration date.
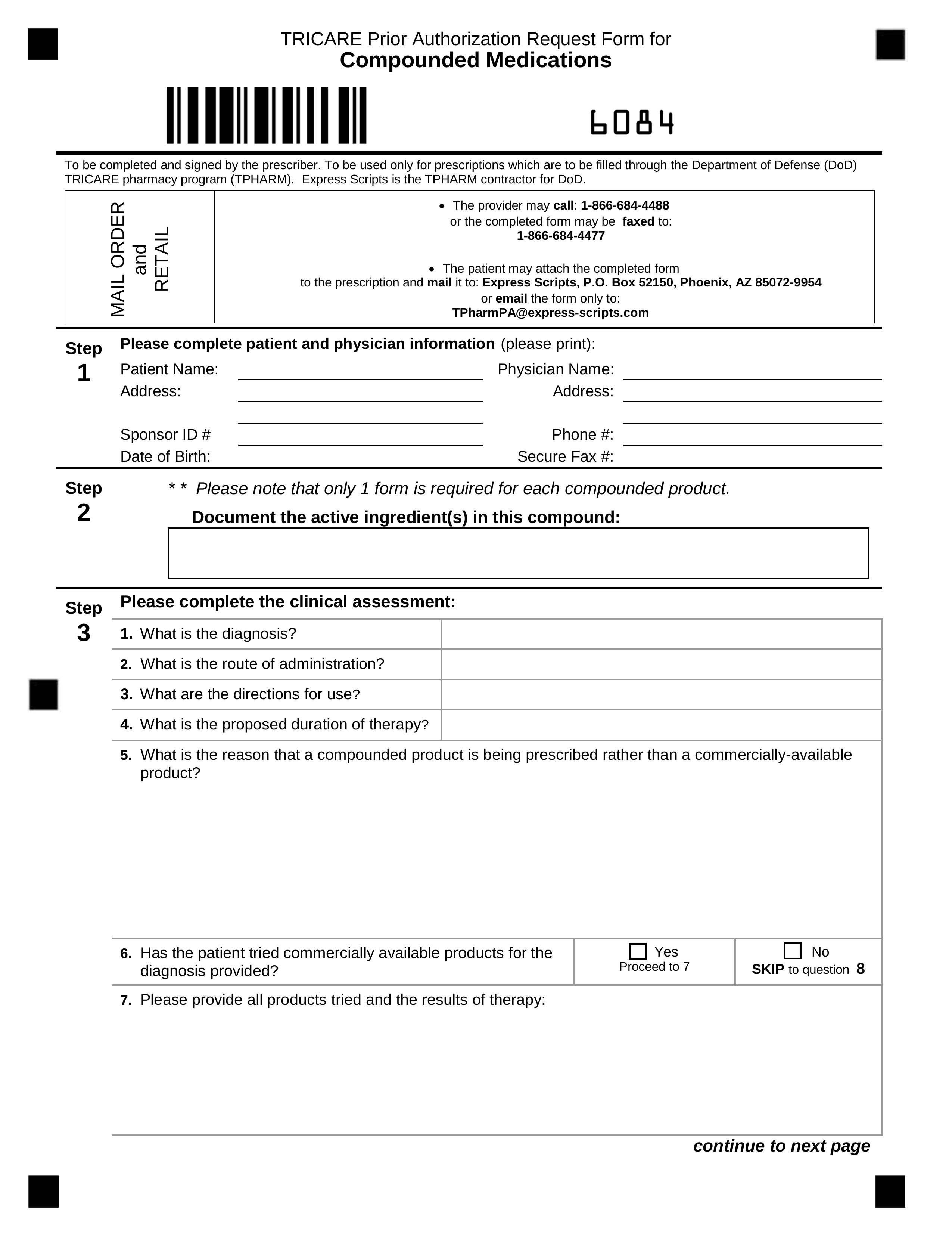
How to Get Prior Authorization. Instructions are on the form. Inpatient TRICARE Service RequestNotification Form.
View your referrals andor authorizations. To allow you to view and manage you and your familys appointments at military hospitals and clinics refill prescriptions and view your personal health data through TRICARE Online. The quickest easiest way to request a new referral or authorization or update an existing referral or authorization is through provider self-service.
Prior authorization is not required for emergency care. Simply select the beneficiarys TRICARE plan option for example TRICARE Prime or TRICARE Prime Remote the beneficiary type for example active duty service member servicing provider type for example network or non-network and the. Youll get an authorization letter after its approved.
Give the form to your provider to complete and send back to Express Scripts. Search the TRICARE Formulary. You can also check the status of your Tricare referral form through the online portal.
For both Generations Advantage and US Family Health Plan members prior authorization may be requested by the members PCP or by the servicing providerfacility. Your records may be disclosed to the Department of Veterans Affairs for determining benefits and providing care as well as to certain other federal agencies to facilitate research and analysis. What does it mean to get prior authorization.
Facilities unable to access the internet can fax the. A TRICARE prior authorization form is a document to be completed by a prescribing physician requesting a specific type of medication for their patient which is otherwise not covered by their TRICARE plan. Use the Prior Authorization Referral and Benefit Tool to find out if a service requires a Health Net referral or prior authorization.
Review the number and frequency of authorized visits. Prior Authorization Referral and Benefit Tool Coronavirus COVID-19 testing reminder. Providers should submit referrals and authorizations including behavioral health through self-service.
If you have a referral then your provider gets prior authorization at the same time. If you have not done so already you will need to register for secure services. If the specialty provider recommends surgery or other procedures you need to go back to your PCM or regional contractor to get another referral and a new authorization.
This tool is for outpatient requests only. Be aware there some services require a separate prior authorization review. Schedule your appointment with the TRICARE provider listed in the authorization letter or contact your regional contractor if you need to find another provider.
You dont need to send multiple forms. Learn more about the Genetic Molecular Lab Testing Notification Prior Authorization Process. If youre not required to get referrals you should know what services need prior authorization.
You can check on your. Use without website registration. Search for your drug on the TRICARE Formulary Search Tool.
Check the TRICARE Formulary to see if you need prior authorization. Labs must register their tests to participate as part of the Genetic and Molecular Lab Testing NotificationPrior Authorization process.


