Massachusetts Standard Form for Medication Prior Authorization Requests eForm or contact Clinical Pharmacy Operations. Blue Advantage Drug Prior Authorization.
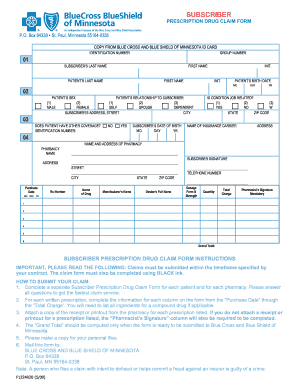 Mnbcbs Fill Out And Sign Printable Pdf Template Signnow
Mnbcbs Fill Out And Sign Printable Pdf Template Signnow
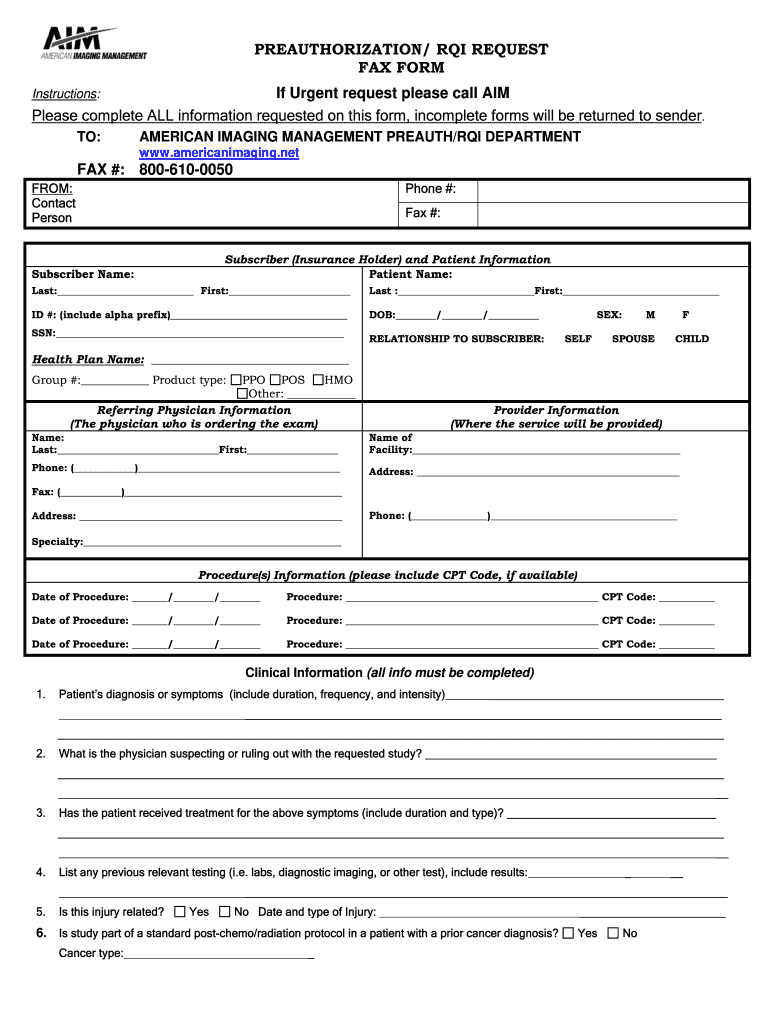
Medical policy precertification and preauthorization router.
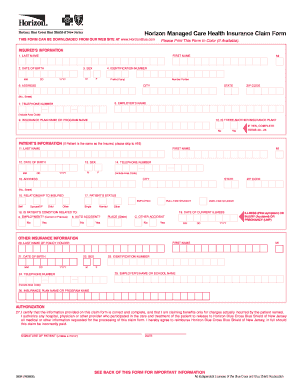
Bcbs of new jersey prior authorization form. Here are the steps you can take as a member if you find a prescription requires prior authorization. 1 2021 Blue Cross and Blue Shield of Texas BCBSTX will update its list of Current Procedural Terminology CPT codes requiring prior authorization to comply with changes as a result of new replaced or removed codes implemented by the American Medical Association. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts.
Blue Cross Medical Record Routing Form PDF Commercial. Authorization for Disclosure of Mental Health Clinical Information. Provider resources for New Jersey Community Plan products including prior authorization information provider manuals forms recent news and more.
Also known as preauthorization or pre-notification pre-certification confirms that a physicians plan of treatment meets medical necessity criteria under the applicable health benefit plan. To find a prior authorization form visit our forms page or click on the links below. Contact the prescribing physician and let them know that your medication requires a prior authorization.
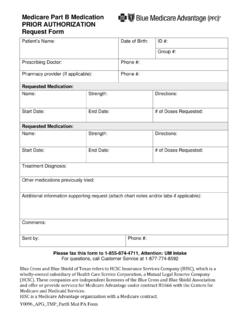
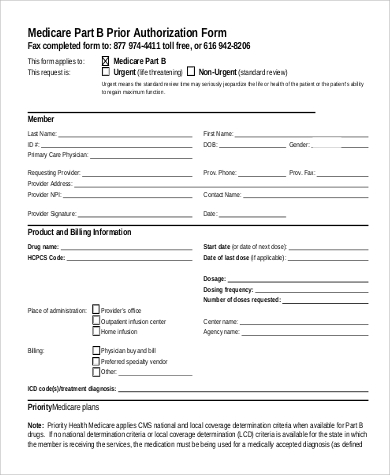
Medical Policy and Pre-certificationPre-authorization for Out-of-Area Members Whats New. Non-formulary drugs Part D reviewed by ESI. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
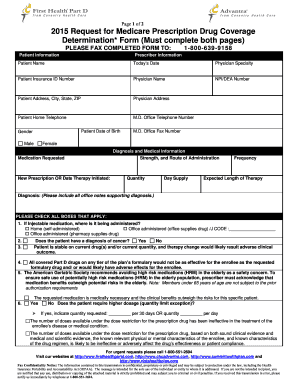
Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB. Use this form to request authorization by fax or mail when a n issuer requires prior authorization of a health care service. NYS Medicaid Prior Authorization Form for Prescriptions.
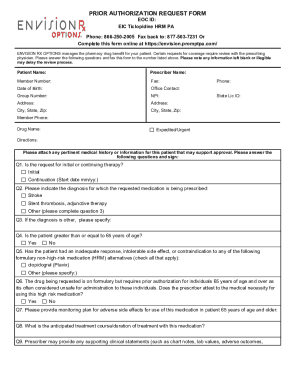
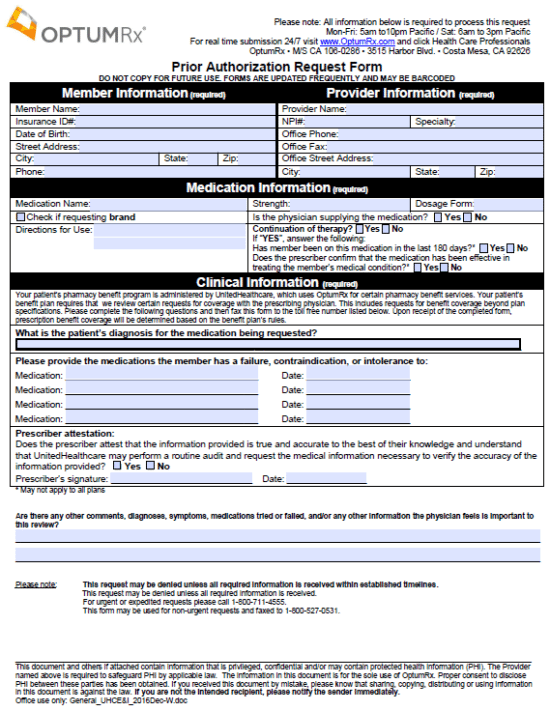
To request prior authorization for these medications please submit the. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. GENERAL INFORMATION Patient Name Request Type please check one Prior Authorization Step Therapy Exception Request for Quantity Limit Exception City Appeal Mandatory Generic Exception Request for Non-Formulary Exception.
To 5 pm Eastern Time. Waiving Pre-CertificationPrior Authorization requirements for acute inpatient facility admissions Waiving Pre-CertificationPrior Authorization requirements for acute inpatient facility admissions Providing Telephonic care with no costs to members Providing Telephonic care with. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Blue Advantage Physician Drug Authorization Request Form. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out.
Behavioral Health Substance Abuse Certification. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Provider Forms Guides Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location.
Other medications that require prior authorization. Behavioral Health Case Management Prescreening. Requests for the following services can be made by fax or mail.
Ask how long it usually takes for your physician to complete the appropriate forms to initiate the prior authorization process. Blue Choice members using their self-referred benefit do not need to get prior authorization. Most PPO benefit plans require the member or provider to pre-certify inpatient hospital admissions acute care inpatient rehab etc.
Behavioral Health Substance Abuse Continued Stay Review Form. An Issuer may also provide an electronic version of this form on its website that you can complete and submit electronically through the issuers portal to request prior authorization of a health care service. Out of Plan Referral Review Request Form This form is used to request an Out-of-Plan Referral also referred to as an Out-of-Network Referral for services outside of the Servicing Network.
If you have questions about this tool please call your Network Specialist at 1-800-624-1110 at the prompt select More Options and then Network Relations weekdays from 8 am. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. We are currently in the process of enhancing this forms library.
Plans supported include NJ FamilyCare and UnitedHealthcare Dual Complete ONE. Acute Inpatient Fax Assessment Form PDF Acute Rehabilitation and Skilled Nursing Facility Assessment Form PDF Benefit Enhancement Assessment Form PDF LTACH and Skilled Nursing Facility Enhancement Assessment Form PDF Blue Cross PPO Request for Preauthorization Form. The Prior Authorization Procedure Search tool helps you determine if services require prior authorization for your Horizon BCBSNJ patients.