Fax completed forms to FutureScripts at 1-888-671-5285 for review. If we determine that the services are medically necessary we send an approvalor authorizationin writing to the member primary care provider PCP the treating physician and the facility if applicable to let them know that we have approved the services.
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
Urgentemergency admissions do not require prior authorization.
Blue cross blue shield prior authorization. Get a Free Quote. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Outside the United States.
Members and providers are encouraged to obtain prior authorization and may call Customer Service to inquire about the need for prior authorization. In the United States Puerto Rico and US. We review them to ensure they are medically necessary.
If you do not obtain prior approval there may be a reduction or denial of your benefit. This is called prior approval precertification or preauthorization. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Prior Authorization of Drugs Upload date. Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad. You will be notified by fax if the request is approved.
This is called a prior authorization. When a request for service is not approved we notify the PCP and the member. While the list below covers the medical services drugs and procedures that require authorization prior to rendering.
Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Prior authorization is required for the medications listed in these policies when administered in a clinicians office or outpatient setting and billed under the members medical benefits. This list will be updated no.
Search for Doctors Hospitals and Dentists Blue Cross Blue Shield members can search for doctors hospitals and dentists. Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad. Medical Utilization Management MED UM Pharmacy Prior Authorization Policy 033 Medical Benefit Prior Authorization Medication List 034.
Certain medical services and treatments need approval before you receive care. Precertification is required for many services including the following outpatient hospital benefits physician benefits and other covered services. Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Prior Authorizations BCBSTX must approve certain covered health services before you get them. Below is the list of specific services in these categories that require precertification.
Make sure you include your office telephone and fax numbers. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan. Blue Cross Blue Shield of Rhode Island is an independent licensee of the Blue Cross and Blue Shield Association.
Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity. Laboratories andor a third party vendors are not allowed are not allowed to obtain clinical authorization or participate in the authorization process on behalf of the ordering physician. Get a Free Quote.
Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members. When completing a prior authorization form be sure to supply all requested information. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required.
Prior authorization requirements apply to all of the HealthSelect plans except HealthSelect SM Secondary. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Once notified of admission medical information is applied against InterQual criteria for level of care review. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Only the ordering physician shall be involved in the authorization appeal or other administrative processes related to prior authorizationmedical necessity.
Blue Shield may require additional information after the service is provided.
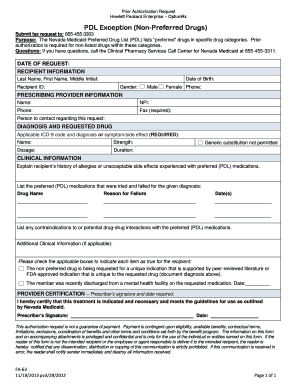 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
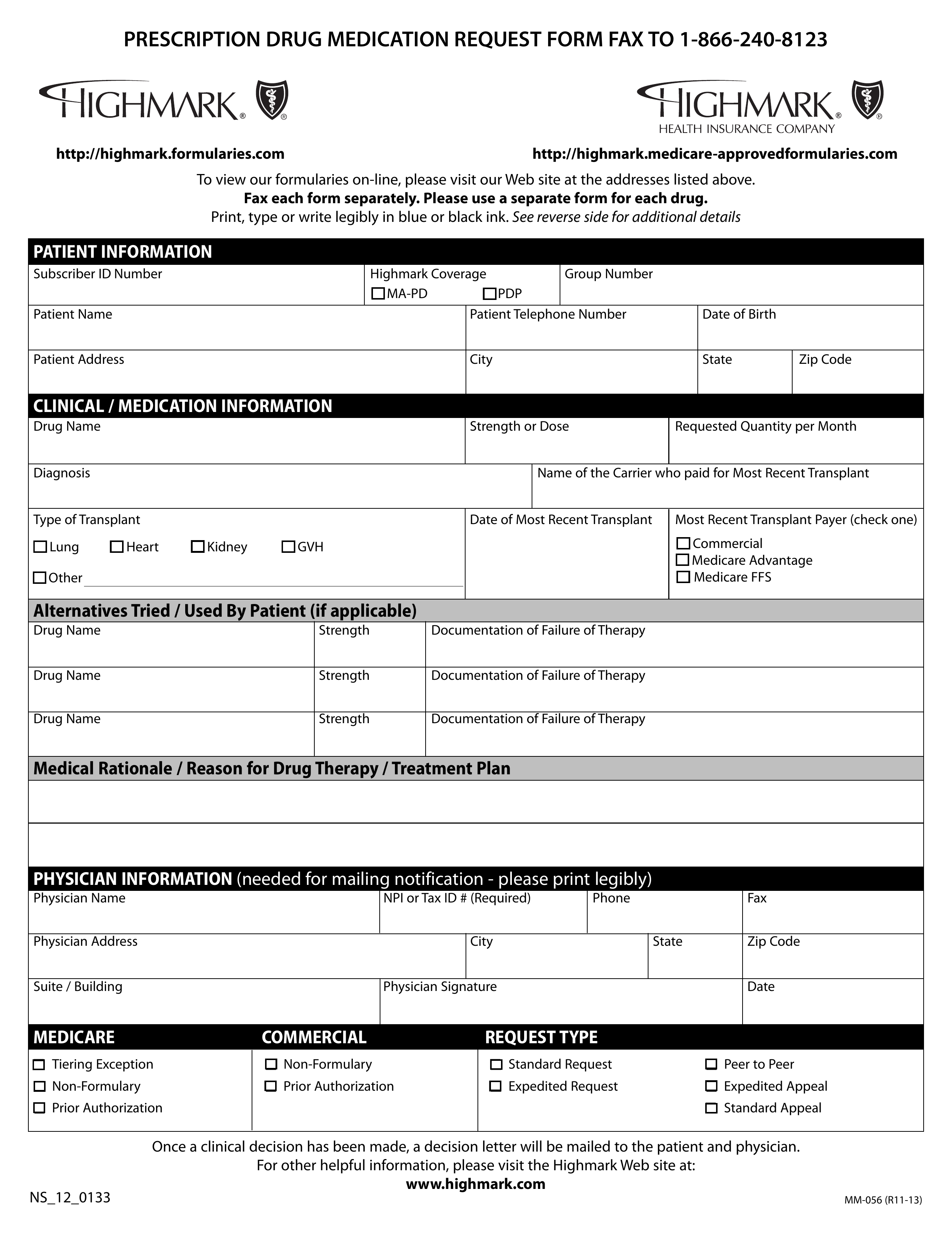 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
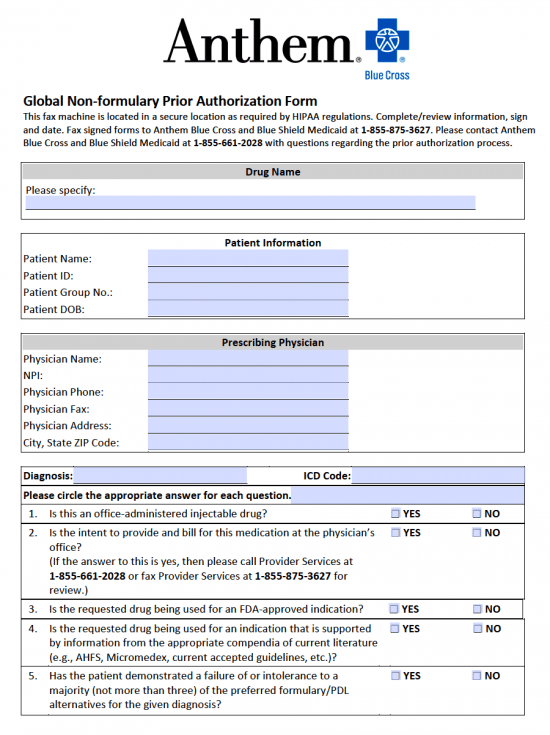 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
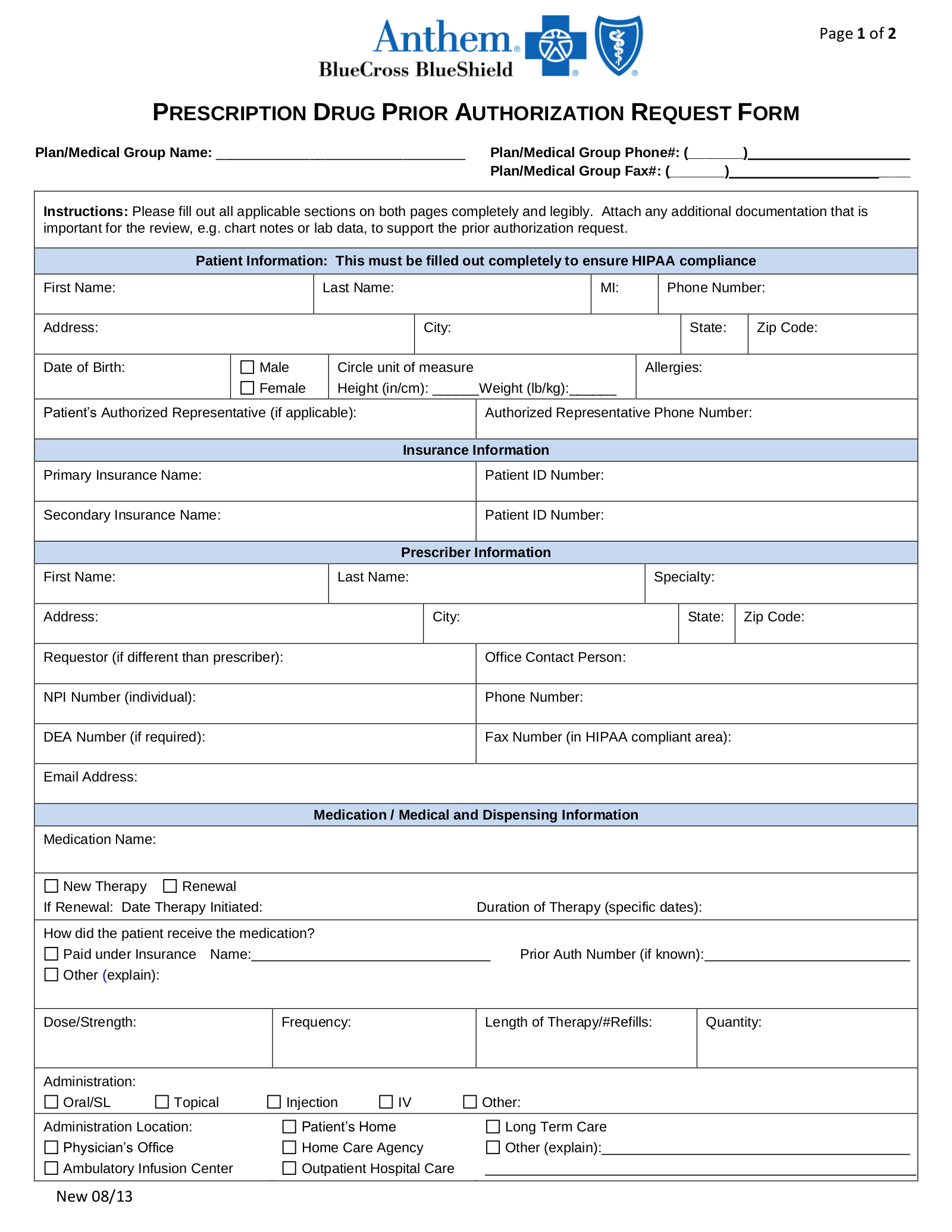 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
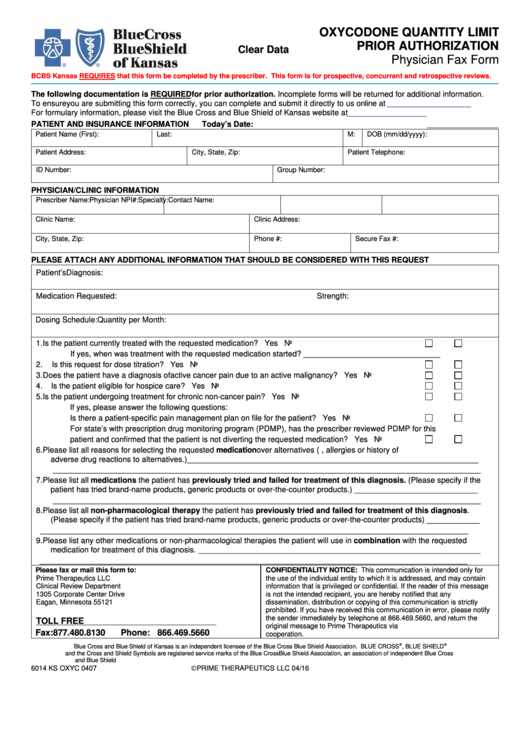
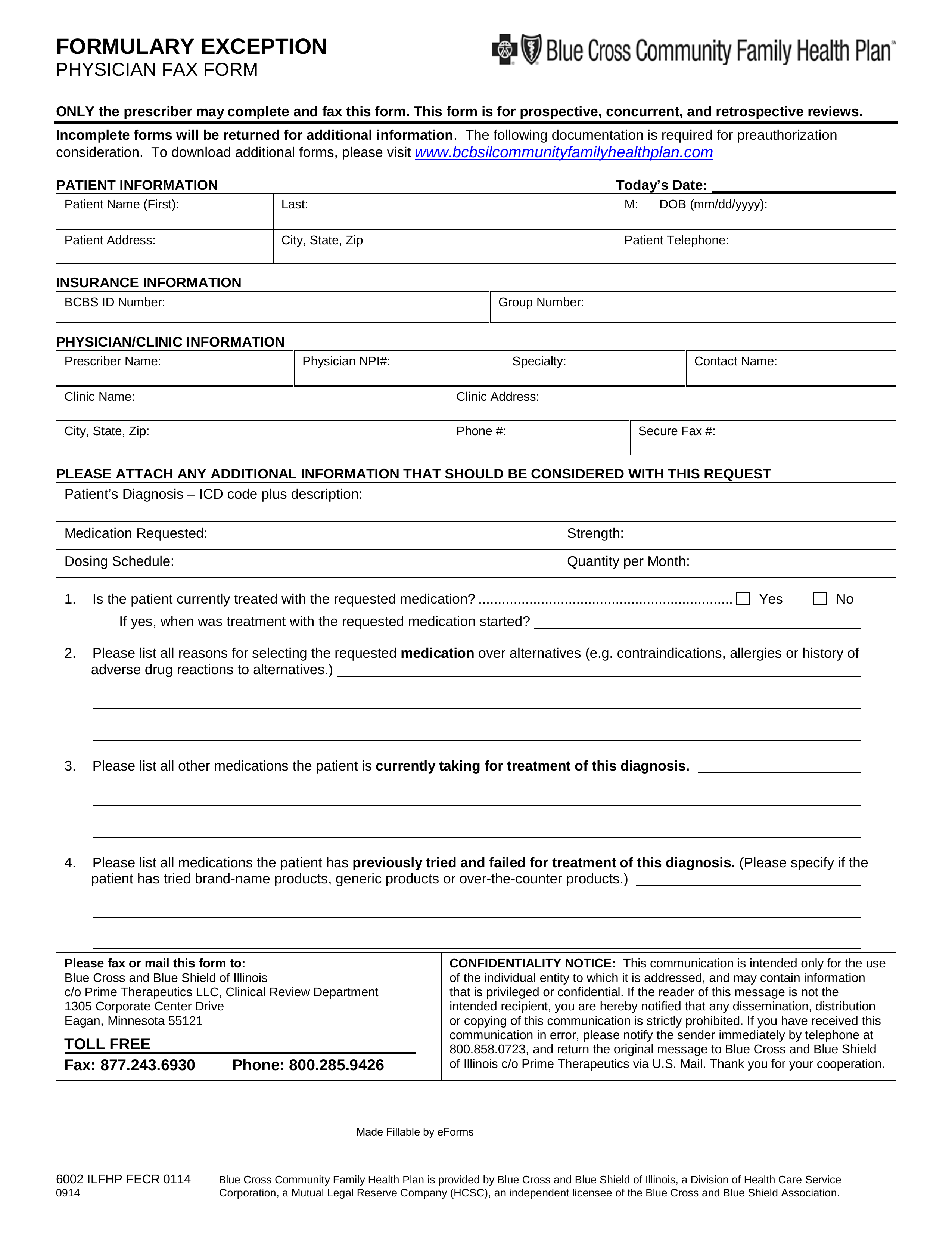 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
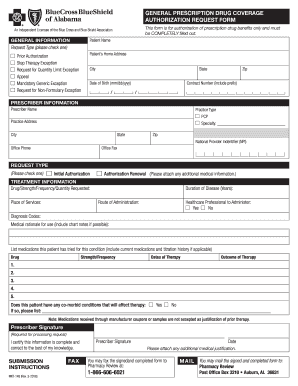 Blue Cross Blue Shield Of Alabama Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Blue Cross Blue Shield Of Alabama Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
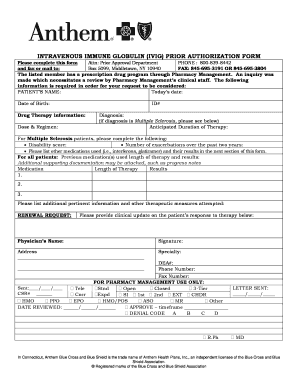 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.