Health insurers are trying to spark a price war by refusing to pay for some brand-name medications unless they get a big discount. Youll pay the remaining 25 of the price.
 Corporate Incentives Make Insurers Favor Pushing Brand Name Drugs Over Cheaper Generics Pacific Standard
Corporate Incentives Make Insurers Favor Pushing Brand Name Drugs Over Cheaper Generics Pacific Standard
We discovered that brand name Synthroid is.

How to get insurance to pay for brand name drug. Synthroid runs between 45 and 67 for 30 pills. What drugs require step therapy. You are right that it is more expensive than the generic medication.
Prescription formularies are developed based on efficacy safety and cost-effectiveness of the medications. The cost of prescription drugs. Yes but as k.
You and your doctor can either complete and file an appeals form provided by your insurer or write a letter that includes the name of the drug why you need it covered and any other supporting. Some insurance companies do allow coverage for medications prescribed by a doctor which have. Those not listed are referred to as non-preferred drugs.
But with many insurance companies you have to fork over a lot more now than a mere copay or they wait for an event to occur before allowing you to go back on the brand name. Synthroid is a long-standing brand name version of levothyroxine. If the insurance denies the claim your physician will need to recommend a generic equivalent.
The generic version costs between 12 and 16 for the same 30 tablets. The general process for most Insurance Companies to get your drug covered by the Exception process is very simple. Drugs listed in the formulary are known as preferred drugs.
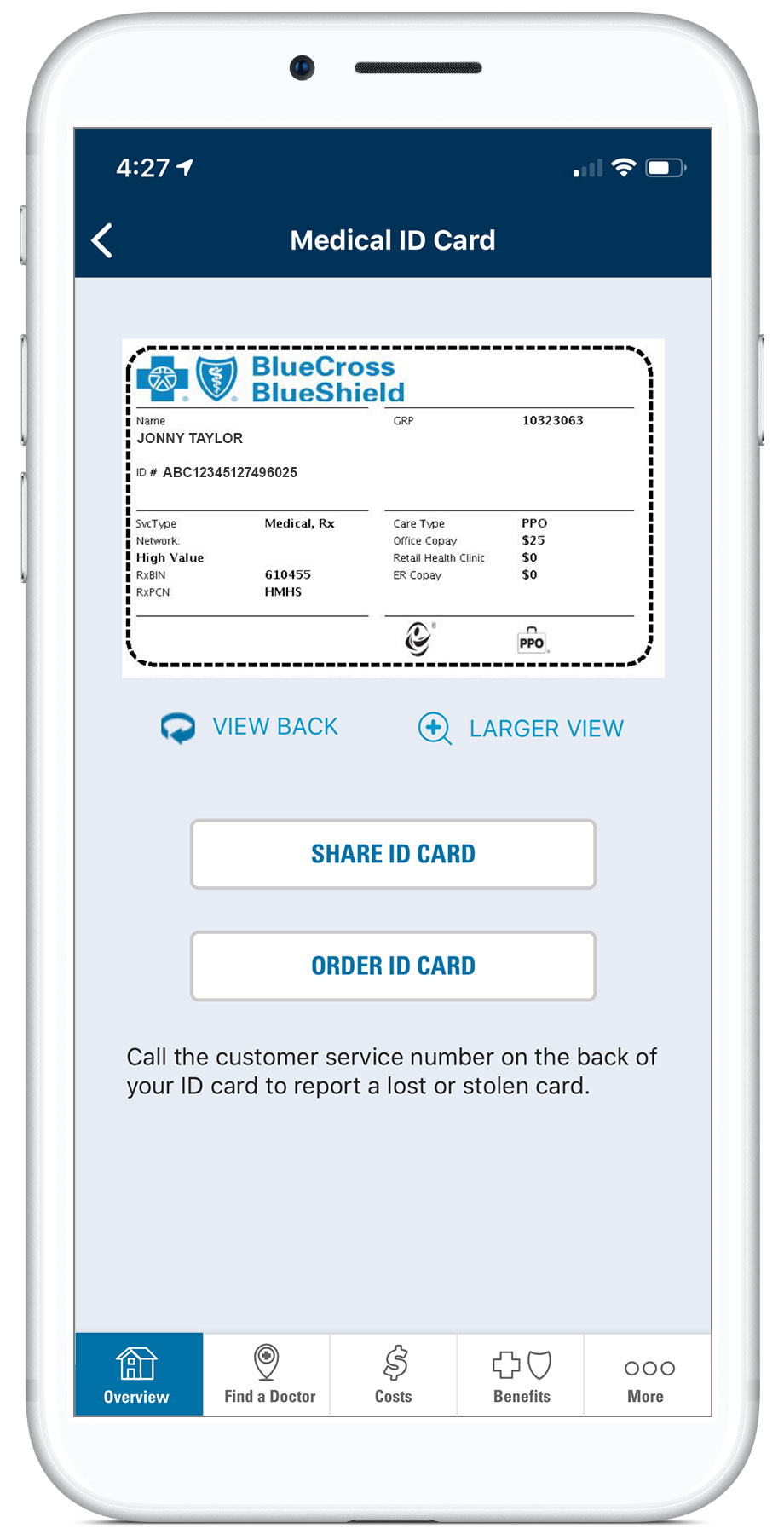
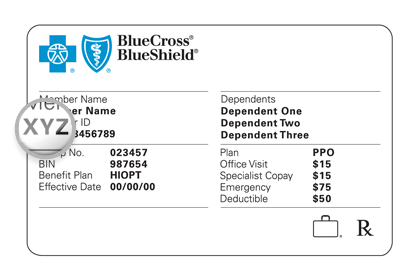
You and your doctor can either complete and file an appeals form provided by your insurer or write a. Your doctor must confirm to your health plan insurer either in writing or orally in person or by phone that the particular drug you require is appropriate for your medical condition based on the following criteria. I live in Georgia and we are currently looking at Blue CrossBlue Shield and Humana.
For generic drugs only the amount you pay will count toward getting you out of the coverage gap. This forces some people to change their prescriptions. Health insurance companies typically publish a formulary that lists the drugs both generic and brand name that your plan will cover.
Even if your doc did write the brand name the insurance companies I have had will charge much more for brand names if you dont accept their generic. Wont like it or cover itGood Luck to youdd. You can get Medicare prescription drug coverage through a Medicare Advantage Prescription Drug plan MAPD or a stand-alone Medicare Part D Prescription Drug Plan which works alongside your Original Medicare coverage.
Many have adopted tiered prescription benefit plans with specialty drugs in the fourth tier which has the highest cost-sharing either through co-payments or co-insurance. The price patients eventually pay gets determined later when an insurance company or pharmacy benefits manager decides where a drug fits on a list of covered treatments called a formulary. The discount for brand-name drugs will apply to the remaining amount that you owe.
Insurers and other payers look first at how well the drug works not its cost when they decide whether to cover the latest treatments according to the nations largest pharmacy benefits manager Express Scripts. However the specific prescription drugs covered may vary by plan so its possible that certain prescription drugs you need may not be covered by your Medicare. Some examples of these drugs include Differin Clarinex Abilify Fenoglide Nexium and Prilosec.
Medicare will pay 75 of the price for generic drugs during the coverage gap. Juie 29 Sep 2013. If your insurer still denies your request to cover a drug you need you can file an appeal.
So instead of paying 65 a month for a brand-name drug you might pay only 4 a month with a coupon. Thats why many insurance companies only want to pay for generic levothyroxine. Your doctor may need to explain the reason why the brand name medication is needed.
I might be forced to switch to generic if my doctors appeal to the insurance. Plus only about half. Drugmakers promote coupons as a way to help people afford their medications.
Described you can get brand name- but your insurance. I think there is a process where your doctor can call in and require you to get the brand name. The coverage for generic drugs works differently from the discount for brand-name drugs.
Kaw06 29 Sep 2013. Insurers will typically require step therapy for expensive brand-name drugs that have affordable alternatives but the actual list of drugs will differ plan to plan.