Cover these drugs under certain circumstances. How much is my testosterone co-pay with Medicare.
 Does Medicare Pay For Testosterone Injections
Does Medicare Pay For Testosterone Injections
How Part D works with other insurance.
Does medicare part d cover testosterone. Side effects of testosterone include worsening of sleep apnea decreased HDL and polycythemia. Find affordable quality Medicare insurance plans that meet your needs. Costs for Medicare drug coverage.
Some Medicare plans have restrictions on coverage of testosterone cypionate that may include. Symptoms of Low Testosterone Levels. Medicare Part D Prescription Drug Coverage.
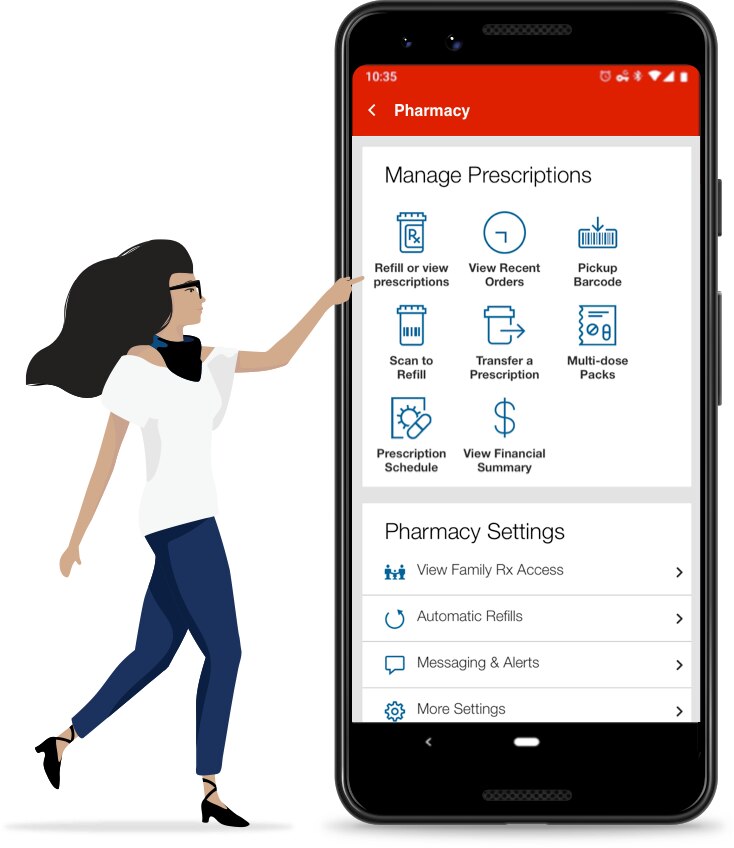
Anzeige Find your best rate from over 4700 Medicare plans nationwide. A persons Medicare drug plan Part D may. Prior Authorization Most Medicare plans will require you to obtain their authorization before they will provide coverage for this prescription.
He or she should call the plan for more information. Careful monitoring of testosterone levels should occur every 3-6 months. Medicare coverage for many tests items and services depends on where you live.
The formulary might not include your specific drug. A person might need to pay out-of-pocket for these drugs and submit a claim to their Part D plan to get paid back. If your test item or service isnt listed talk to your doctor or other health care provider.
In order for Medicare benefits to cover testosterone pellets certain requirements must be met. Anzeige Find your best rate from over 4700 Medicare plans nationwide. Learn about formularies tiers of coverage name brand and generic drug coverage.
A Medicare Advantage plan is provided by private health insurance companies so depending on the plan. 65 of Medicare Part D and Medicare Advantage plans cover this drug. 767 Zeilen If you are enrolled in a Medicare plan with Part D prescription drug coverage you.
On average testosterone levels are expected to decrease slightly as men age but some men may experience drastically lower testosterone levels at different points in their lives. All Medicare drug plans generally must cover at least 2 drugs per drug category but plans can choose which drugs covered by Part D they will offer. Find affordable quality Medicare insurance plans that meet your needs.
65 of Medicare Part D and Medicare Advantage plans cover this drug. Overview of what Medicare drug plans cover. The coverage is optional and offered by private insurance companies approved by Medicare.
MEDICARE PART D COVERAGE CRITERIA ANDROGEL testosterone Plan Limitations. This list only includes tests items and services that are covered no matter where you live. Learn about how Medicare Part D drug coverage works with other coverage like employer or union health coverage.
Levels of testosterone peak in men around the time they turn 19. Original Medicare Part A and Part B typically does not cover hormone replacement therapy. Hematocrit should be checked prior to starting at 3 6 months then annually.
04162021 5 min read Summary. However Medicare Advantage or Medicare Part D may cover the cost of hormone replacement therapy drugs. Some Medicare plans have restrictions on coverage of testosterone cypionate that may include.
TOM trial was discontinued early because of increased rate of CV events. Learn about the types of costs youll pay in a Medicare drug plan. Applies to all Blue Shield of California Medicare Part D plans.
However in most cases a similar drug should be available. Some of these can include your testosterone levels being below a certain level having a confirmed medical diagnosis that is causing the low levels and not taking other supplements that may also boost or lower testosterone levels. If you need Medicare coverage for prescription drugs related to hormone replacement therapy you can consider a Medicare Advantage plan or a Medicare Part D plan that includes coverage for these types of drugs.
Does Medicare Cover Low T Treatment. You can get help paying for medications with a Medicare prescription drug plan under Medicare Part D. The short answer to this question is no Original Medicare Part A and Part B does not cover the cost of hormone replacement therapy HRT.
Prior Authorization Most Medicare plans will require you to obtain their authorization before they will provide coverage for this prescription. How much is my testosterone co-pay with Medicare.