If you have questions contact gateway provider servicing department at 1 800 685 5205. To obtain the payer ID please call 615 869-0030.
 How Do I Find The Payer Id Number Drchrono Customer Success
How Do I Find The Payer Id Number Drchrono Customer Success
It serves as the electronic address so the clearinghouse knows which payerinsurance company to send the claim.
Payer id on insurance card. The responsible party is the policy holder and is where you would put the subscriber id. So check and find yours. If you are unable to locate the payer ID please enter NA or None.
The payer ID is generally five 5 characters but it may be longer. We may occasionally update this brochure during the year. Locate the entries that relate to an Office Ally payer and select the Active Card Count.
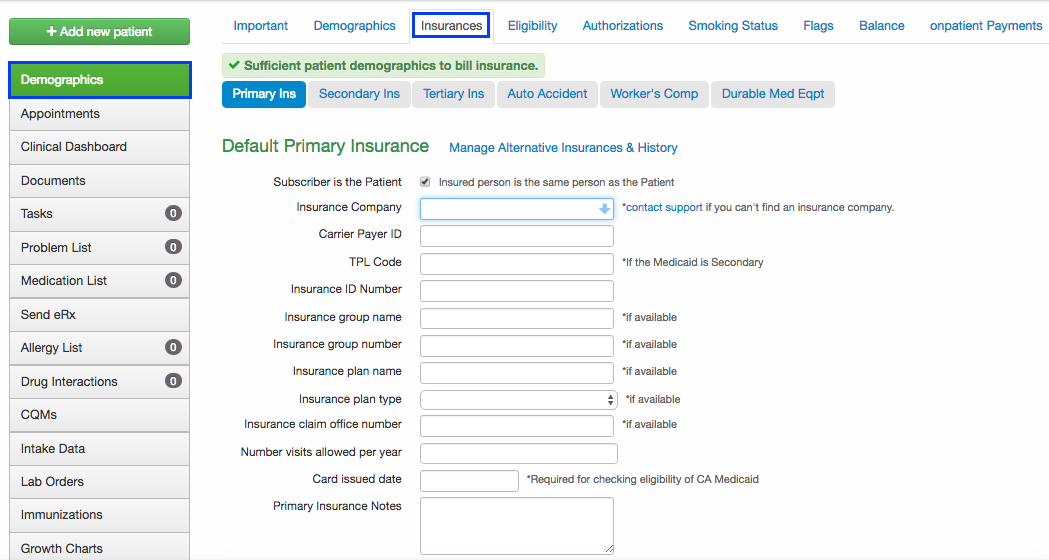
Locate the desired insurance card and click the icon. In the case of a claim rejection the clients member ID card will be the starting point for determining what needs to be corrected. Finally the Payer is who actually makes the payment and is where youd put the PBM routing numbers or payer ids when those become available.
Gateway health plan has several different payer id numbers please look for the payer id on the id card before submitting. If you are finding it difficult to get your policy number on insurance card contact your company you will be asked some security questions. A Payer ID is a unique ID number that is assigned to an insurance company for the purpose of transmitting your claims electronically.
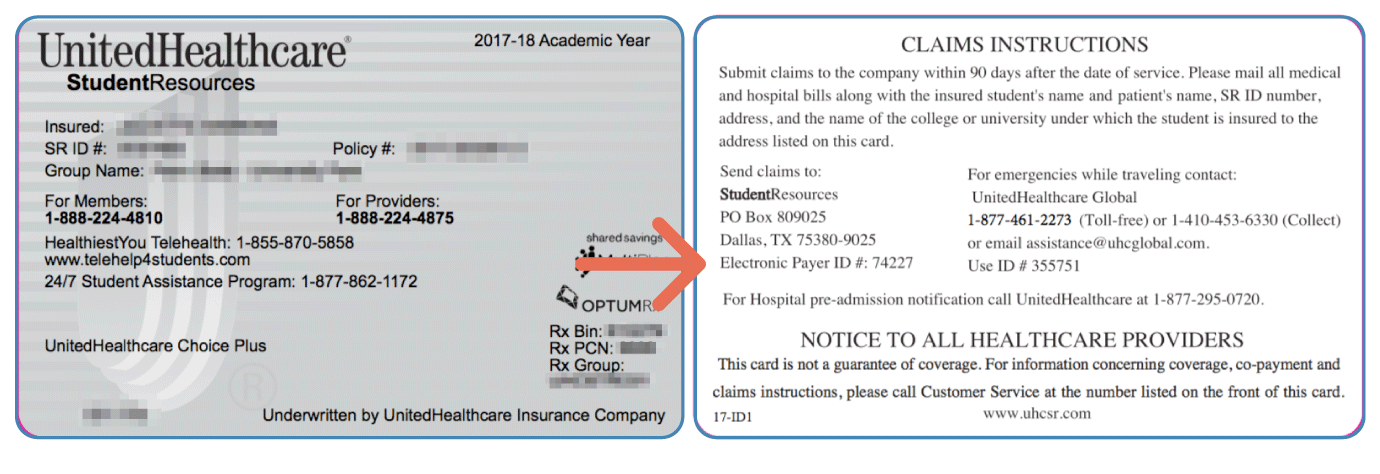
The payer ID is often located on the back of the insurance card in the Provider or Claims Submission section. Some national payers such as Aetna 60054 Cigna 62308 and United Healthcare 87726 have universal payer ids that can be used across all clearinghouses. 2734 rijen The Insurance Payer ID is a unique identification number assigned to.
PA Medicaid 25169Green Card. Insurance card on file. It can also be listed under numerous headers such as Member ID ID or Membership.
Your member ID could be anywhere from 5-12 digits long and should be listed on your health insurance card. If you are not the policyholder then your card may show your name and the policyholders name in separate fields. PHYSICIANS ACCOUNTABLE CARE ORG.
It may also be alpha numeric or a combination. Each person covered by a health insurance plan has a unique ID number that allows healthcare providers and their staff to verify coverage and arrange payment for services. Your policy number is the same as member id or subscriber id number.
Start by looking at your clients insurance member ID card to see if there is a payer ID listed on it. Payer ID only valid for ID cards referencing this payer id. We highly recommended uploading copies of the front and back sides of your clients insurance member ID cards.
The Payer ID on an electronically submitted claim tells the clearinghouse where to deliver the electronic claim file. In the Policy Info section enter the name or Payer ID into the Ins Company field and select the corresponding payer that has AV listed at the end. You can find your Member ID listed on your health insurance card on your e-health portal or by calling your insurance provider.
Please enter Group Number from ID card when submitting claims. Payer id number on insurance card blue cross. Check your health insurance ID card.
Each company has a specific number and it must be entered correctly in the patients chart in order to successfully transmit the claim to the clearinghouse and to the payer. Each payer or insurance has its own payer id number to accept electronic claims. For example the back of this member ID card includes the Electronic Payer ID 74227 - this is.
The Payer ID is assigned to the insurance carrier by the clearinghouse and is not necessarily the same number as found on the patients insurance cards. For example the Payer ID for Insurance Company X may be 12345 with Clearinghouse A and 67890 with Clearinghouse B. Below are some common examples.
Gateway Health Plan has several different Payer ID numbers please look for the Payer ID on the ID card before submitting. Contact your insurance company. It can also help you understand the requirements associated with our various plans allowing you to quickly and efficiently serve your patients.
To locate the appropriate payer ID. You should always look up your Payer ID on the clearinghouses payer list to ensure that you are sending to the correct insurance Links are provided below for easy access. On the Client List click the next to each client name.
If you have questions contact Gateway Provider Servicing Department at 1-800-685-5205. This brochure can help define and clarify information that appears on Cignas most common customer ID cards. Payer IDs are unique to each insurance payer and often times they are clearinghouse-specific.
The identifier associated with them is where you put the member id.