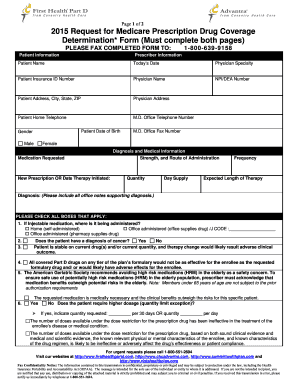
Fax number if a decision letter by fax is requested If you would like to receive your decision letter by fax enter your 10-digit fax number XXX-XXX-XXXX. Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare.
 Advantra Silver Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
Advantra Silver Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
TTY 1-877-486-2048 Mailing address.
Medicare prior authorization fax number. However you can still use the Prior Authorization and Notification tool on Link to submit requests for these members. Providers who plan to perform both the trial and permanent implantation procedures using CPT code. 866 504-7262 Member Information Plan.
If you wish to request a Medicare Part Determination Prior Authorization or Exception request please see your plans website for the appropriate form and instructions on how to submit your request. Santa Ana CA 92799. Call your plan or check on their website to look up the proper mailing address or fax number.
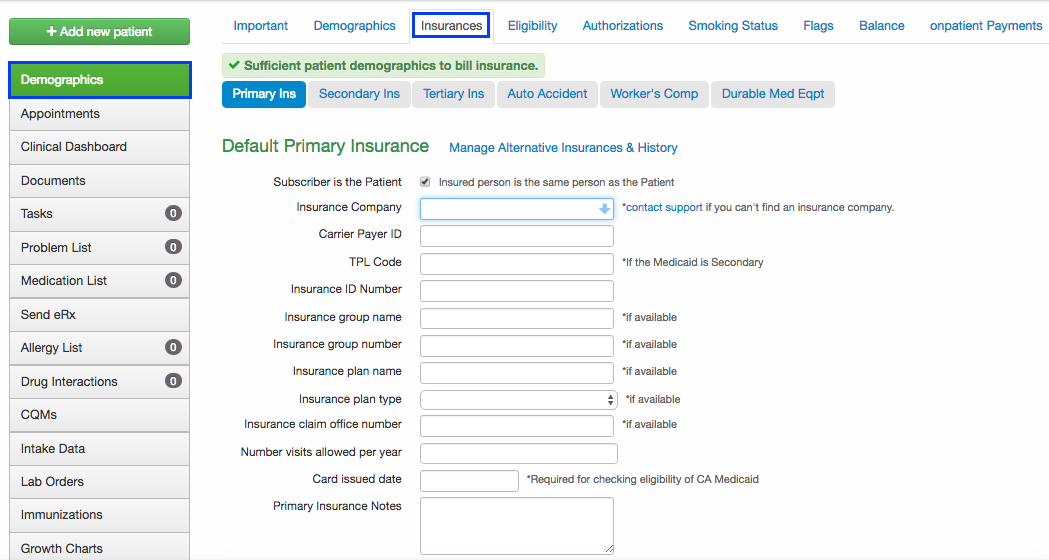
Fallon Health phone and fax numbers Provider Phone Number. Members ID. How can we help.
Medicare Plus BlueSM PPO Preauthorization Fax Process CF 12789 JUL 17 2 R070473 rd. The Standardized Prior Authorization Request Form is not intended to replace payer specific prior authorization. For most plans please use the Prior Authorization and Notification tool on Link.
Send prior authorization forms to the new fax number listed on the authorization form or use the Provider Portal. Complete the appropriate WellCare notification or authorization form for Medicare. Medicare Contact Center Operations PO Box 1270 Lawrence KS 66044.
If the physician feels the request is an emergency situation an expedited review of 24 hours should take place. Prior Authorization is about cost-savings not care. As part of Medicare youll rarely need to obtain prior authorization.
1-844-403-1028 Prior Authorization Department. Molina MedicaidCHIP Molina Medicare Other. The form must be mailed in or faxed directly to your plans office.
Fax numbers are only available for the commercial plans listed below. 866 472-0589 Medicare Fax Number. You dont typically need to get a Medicare prior authorization form as your doctor provider or pharmacist should be able to submit the form to Medicare on your behalf.
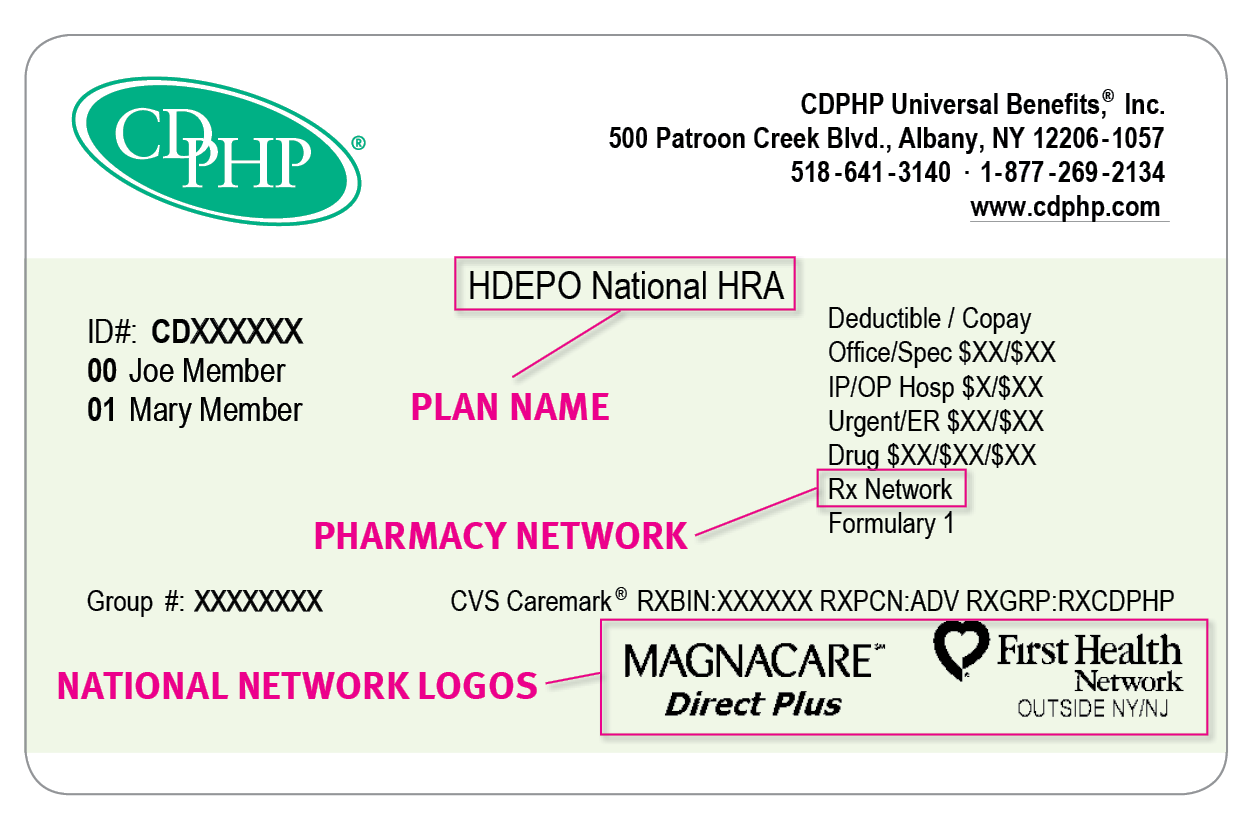
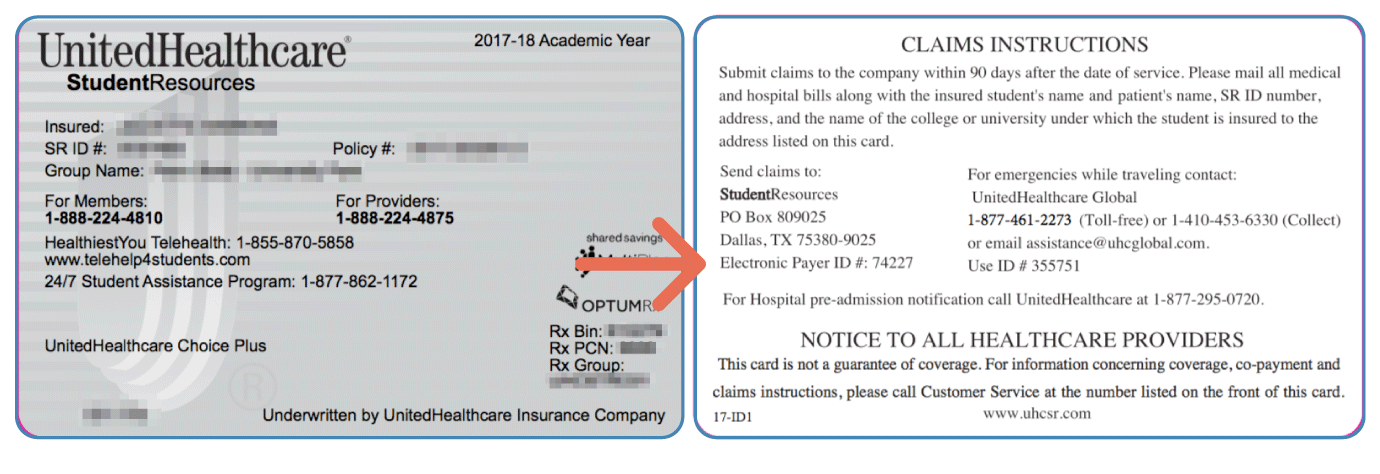
Medical Review - Prior Authorization Requests PAR. You may also ask us for a coverage determination by calling the member services number on the back of your ID card. 1-508-368-9700 Care Review Urgent Fax.
The only service that will require prior authorization for implanted spinal neurostimulators is CPT code 63650. If youre unable to use Link call Provider Services at 8778423210 to submit a request by phone. 888 483-0760 MedicaidCHIP Fax Number.
REQUEST FOR MEDICARE PRESCRIPTION DRUG COVERAGE DETERMINATION. Prior authorization is a type of rule that requires a health care provider to get approval from Medicare before delivering a particular service prescription drug or item to a beneficiary. Massachusetts Nevada and Texas commercial plans are excluded due to state requirements.
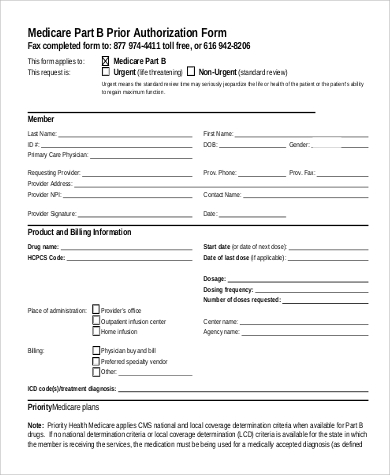
Enter the full name of the individual submitting the prior authorization fax mail cover sheet and required medical records. 1-866-275-3247 Care Review Fax. Medicare Part B Prior Authorization.
701-277-7892 Provider Outreach and Education POE. If a member had greater than 90 days oxygen use pre-authorization would be required effective August 1 2020. Fax the completed forms and any supporting documentation to the fax number listed on the form.
If you want Medicare to be able to give your personal information to someone other than you you need to fill out an Authorization to Disclose Personal Health Information Get this form in Spanish. Plans must respond within 72 hours of receiving your request form. Although some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form.
A copy of the letter will also be mailed to you. Molina HealthcareMolina Medicare Prior Authorization Request Form Phone Number. CMS is temporarily removing CPT codes 63685 and 63688 from the list of OPD services that require prior authorization.
Your doctor will provide this form. Private for-profit plans often require Prior Authorization. For example if a member started oxygen on July 1 2020 pre-authorization would be required starting with the 4th month which is not until October 1 2020.
Optima Medicare and Medicaid Authorizations Government Programs. You can find these forms by selecting Providers from the navigation bar on this page then selecting Forms from the Medicare sub-menu. Commercial plans in Massachusetts Nevada and Texas only.
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. 701-277-7891 Medicare Secondary Payer MSP Inquiries and Refunds. This form may be sent to us by mail or fax.
Part B covers the administration of certain drugs when given in an outpatient setting. Call us at 855-442-9900. Medicare Advantage MA plans also often require prior.
If we approve the admission initial preauthorization request or extension Blue Cross will complete and e-fax a face sheet to the facility indicating the authorization number approved length of stay and last covered day. You have the right to request an organization determination if you want us to provide or pay for an item or.