65000 providers in our. The coverage your plan offers for in-network and out-of-network health care providers and the network your provider is in both impact how much you pay for care.
 What S The Difference Between An In Network And Out Of Network Provider Arc Benefit Solutions
What S The Difference Between An In Network And Out Of Network Provider Arc Benefit Solutions
There are two types of TRICARE-authorized providers.

In network provider. Find a provider by doing. The option is here. This will show you the Network Connections interface.
So an in-network provider also called a preferred provider or participating provider is a medical professional who will offer service to all of the members of your plan at a fixed rate set by an agreement with your insurance carrier. Finding an in-network provider can be done by contacting the doctor or clinic the patient wishes to see. Youll see the menu bar unhide itself.
To unhide it tap the Alt key. What Are the Advantages of Staying In-Network. Insurance companies ask providers if they will charge agreed upon rates for specific services.
When a covered individual goes to an in-network provider the fee for service is billed to the insurance company at the discounted rate specified in the contract with the insurance company. Network so first youll. Network providers are the doctors and other health care professionals medical groups hospitals and other health care facilities that have an agreement with us to accept our payment and your cost-sharing amount as pay ment in full.
Provider Office and Website. This shows you the Advanced Settings dialog. A provider network is a list of health-care providers who are contracted by an insurance company and provide medical care to those enrolled in plans offered by that insurance company.
Insured individuals usually pay less when using an in-network provider because those networks provide services at lower cost to the insurance companies with which they have contracts. Click here for additional details or click on image for more information. If they have a website insurance information is usually listed there.
In network refers to providers or health care facilities that are part of a health plans network of providers with which it has negotiated a discount. There are some exception to this. Dictcc Übersetzungen für network provider im Englisch-Deutsch-Wörterbuch mit echten Sprachaufnahmen Illustrationen Beugungsformen.
When you go to a doctor or provider who doesnt take your plan we say theyre out of network. With a provider network this comprehensive more than 1 million physicians as well as provider facilities hospitals and other care centers most of your care needs are covered in-network which means savings for you. Whether you need care here in the United States or abroad youll have access to health care in more than 190 countries.
The covered individual pays out-of-pocket per the negotiated copay or. We also call them participating providers. In short networks are created by insurance companies.
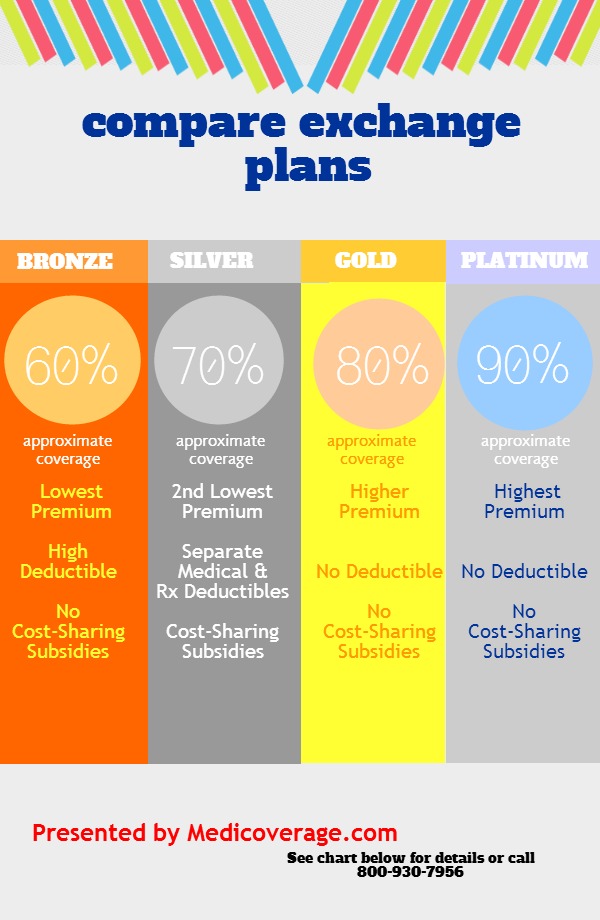
Several insurance companies offer a variety of options with slightly different names and varying coverage levels. Now click the Advanced menu and you can select Advanced Settings. Dieser versorgt den Endverbraucher zum Beispiel mit einem Telefon- Internet- oder.
Ein Provider ist allgemein ein Versorger. If the providers agree to these rates they can be called an in-network provider If the providers do not agree to join the network the health insurance company will label them out-of-network. This is where you can alter the PIN of the SIM card and specify a network provider useful close to borders to avoid expensive roaming as well as select the GSM transfer rate and the reset time including the interval for the GSM module in the ZDUE-GSM-PLUS-V or ZDUE-GPRS-PLUS-IV.
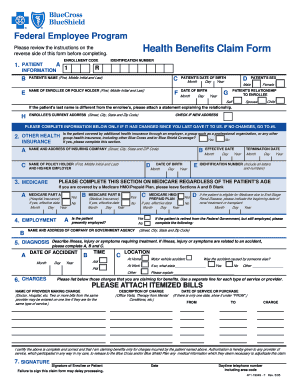
We take the below insurancesbenefit programs. Now you can modify the order by clicking any of the providers and then. The one youd like to see.
Have to narrow it down to. The providers in the health insurance plans network are called network providers or in-network providers. We also call them participating providers.
If you have an HMO plan you are only covered for in-network care except in medical emergencies when. When a doctor hospital or other provider accepts your health insurance plan we say theyre in network. Although Small Town Counseling is primarily an out-of-network provider.
Meistens handelt es sich um den Mobilfunk- oder Internet-Provider. Network Providers Any TRICARE-authorized provider An authorized provider is any individual institutionorganization or supplier that is licensed by a state accredited by national organization or meets other standards of the medical community and is certified to provide benefits under TRICARE. Be sure to look for the exact name of your plan as listed on your ID card.
This term could apply to doctors medical facilities and other types of health-care providers. Now click the Provider Order tab. An in-network provider will bill your health plan directly collecting only the copay or deductible amount from you at the time of services for coinsurance which is a percentage of the total amountrather than a flat rate like the copay and deductibleits generally better to ask the provider to bill the insurance first and then your bill will be determined based on a percentage of the negotiated.