Out-of-Network Prior Authorization Request Form Medica requires that providers obtain prior authorization before rendering services. If you have cards that look like the ones you see here you could get extra help plus things like dental vision and everyday needs like toothpaste and cold medicine with BlueCare Plus our Dual Eligible Special Needs Plan DSNP.
Https Www Bcbsm Com Content Dam Public Providers Documents Global Medication Authorization Request Form Pdf
Sterilization Consent Form English Sterilization Consent Form Spanish Types of Coverage.
Bluecare plus prior authorization form. BlueCare Plus POS members may self-refer to participating and non-participating providers. Blue Cross Federal Employee Program Use these forms to obtain prior authorization for administering medications in physicians offices and outpatient hospitals including urgent care. Medicare with Medicaid BlueCare Plus Forms See all documents forms Review our manuals policies and guidelines to see how we deliver member benefits determine medical necessity and make other important decisions.
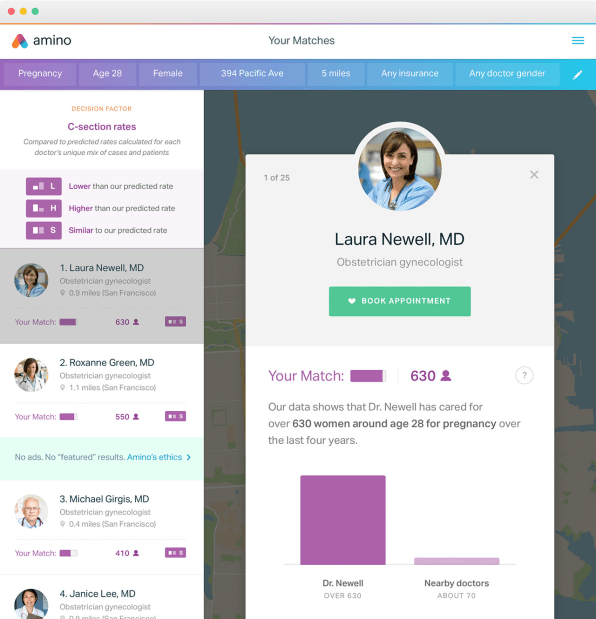
You can download the Physician Request for Prior Authorization form also called the Formulary Exception form. We help 14 million physicians make the best prescribing decisions by providing a more complete view of the patient enabling greater opportunities for whole person health. Please include ALL pertinent clinical information with your Medical or Pharmacy Prior Authorization request submission.
Provider Forms Guides. Sterilization Consent Form Instructions. The provider will have 60 days from the date of the claim denial to.
These plans will generally cover drugs listed in our formulary as long as. We are currently in the process of enhancing this forms library. In most cases our certified pharmacy technicians will be able to take the clinical information right over the phone so please be ready to answer some questions related.
This list shows prescription medications that require your doctor to obtain authorization from us. Want to learn more about TennCare SM CoverKids or the other programs we offer. During this time you can still find all forms and guides on our legacy site.
See if BlueCare Plus is right for you. Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts. The drug is medically necessary.
Prior Authorization Request Form. You can also use CoverMyMeds to request authorization. These forms are also available along with others on BCNs Forms page within Provider Secured Services.
Please contact our Customer Contact Center at 1-888-873-9200 to obtain the appropriate drug specific form. Medicare Plus Blue PPO and Prescription Blue PDP plans include prescription drug coverage. Health Care Providers.
If you are unable to locate the Prior Authorization Request form for the drug youve been prescribed in the list of Prior Authorization Forms available please follow the instructions below based on your province of residence. Prior Authorization Program Information and Authorization Forms PDF To request a prior authorization for a medication included in this program download the appropriate form complete and fax to the number at the bottom of the form. Skilled Nursing FacilityInpatient Rehabilitation Authorization Request.
Authorization requests must be submitted prior to services being providedNote. Plan notification must be submitted prior to services being provided. Request Your Plan Materials.
Below are links to various utilization-management-related forms some of which are used to request authorization for various services. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. However they will be subject to deductibles and coinsurance and to balance billing when care is rendered by a non-participating provider.
Medications that Require Prior Authorization M indicates the pre-authorization is only required for Medex and Blue Care 65 members. Blue Cross Medicare Plus Blue SM PPO Forms. Require plan notification only.
Authorization determinations are conducted for benefit determination or the application of medical necessity criteria or both. The prescription is filled at network retail or mail-order pharmacies. Go to the BCN Advantage medical drug policies and forms page.
See also the notes at the end of Section 1. This list is not all-inclusive. Find helpful details including how to.
TennCare Pharmacy Program co Magellan Health Services 1st floor South 14100 Magellan Plaza Maryland Heights MO 63043 Phone. Must obtain prior written authorization by contacting the Case Management Department at 800 238-2227 toll-free. All other plan rules are followed.
To access the complete Forms Library log in to Provider Secured Services click. After arriving in the provider menu you may either say authorization or select option 1 for prior authorization requests. To ensure that prior authorizations are reviewed promptly submit request with current clinical notes and relevant lab work.
Use these forms to file an appeal about coverage or payment decisions or to file grievance if you have concerns about your plan providers or quality of care. BlueCare Plus PCP Change Form. This is the preferred and most efficient method to generate a medication coverage request.
Magellan Health Services will provide a response within 24 hours upon receipt. Faxed forms with all required information are processed within 10 calendar days from the date received from the provider. Our data-driven tools and technologies help remove barriers to care and offer a simpler better.
If any items on the Medica Prior Authorization list are submitted for payment without obtaining a prior authorization the related claim or claims will be denied as provider liability. Go to the Medicare Advantage PPO medical drug policies and forms page. Fax This Form to.