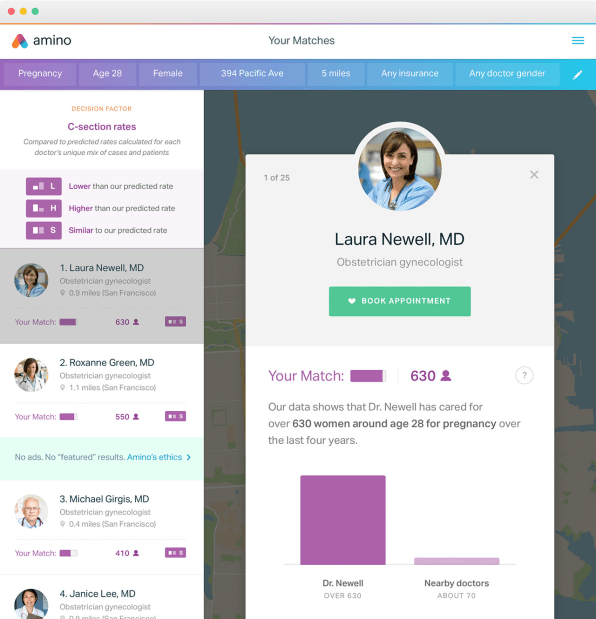
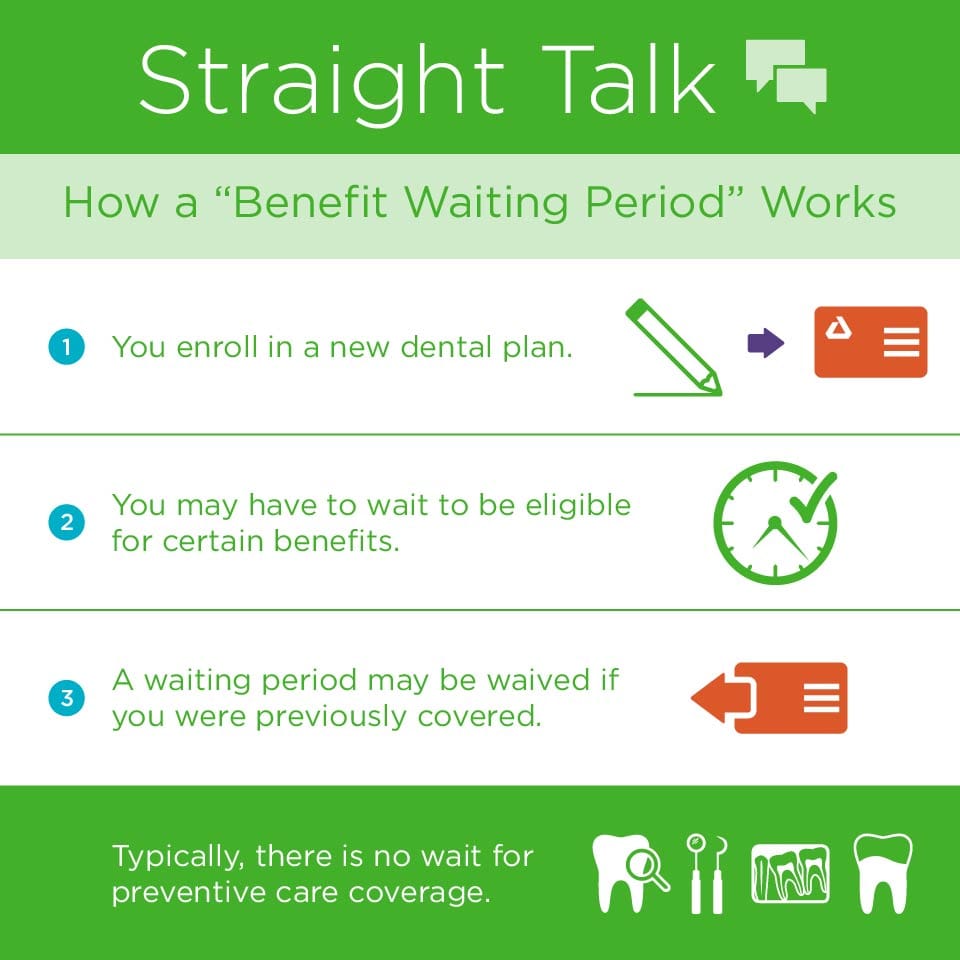
Conversely your dental plan may have a 6- to 12-month waiting period for restorative services such as filings and non-surgical extractions where a 12-month waiting period is often standard for major services such as crowns or dentures. A waiting period is the amount of time that must pass once you are enrolled in your policy before you can use certain benefits in your dental plan.
 Benefit Waiting Periods Delta Dental Of Illinois
Benefit Waiting Periods Delta Dental Of Illinois
Services that often require a 6 month waiting are.

What is a 6 month waiting period dental insurance. Additionally many policies come with long waiting periods for the following types of coverage. They do not want people to wait until they need to get work done then once they need the work to purchase a dental policy and get hundreds or thousands of dollars. A 6-month waiting period applies for implants bridges partial dentures full dentures crowns and cast restorations.
Occlusion adjustment bite adjustment Services that frequently impose a 12 month. How do dental insurance waiting periods benefit you. Dental insurance waiting periods are common with some policies having waiting periods as long as 12 months but there are dental policies that advertise themselves as no waiting period.
A 12-month waiting period applies for initial placement of bridge or denture to replace one or more missing natural teeth. The Private Health Insurance Ombudsman shows some examples of typical waiting periods for major dental procedures like crowns bridges or orthodontics commonly incur waiting periods of up to twelve months. These waiting periods are established to protect the dental insurance companies.
Dental insurance with no waiting periods cost about the same as dental insurance with waiting periods. If you receive services during a waiting period your dental coverage may not pay for them. Maternity care - Usually between 10 to 12 months.
Space maintainers for young children. Fixed partial denture sectioning. Before you can start claiming on your health cover you must have held your cover for a certain amount of time known as a waiting period.
Typical waiting periods are 6 months and 12 months. Though policies vary greatly from provider to provider many dental insurance plans require a waiting period of anywhere from six to 12 months before theyll pay out any benefits for basic services. For example some plans may require a 6-month waiting period for basic restorative services such as fillings and non-surgical extractions.
A typical waiting period for major services could be anywhere from 12 to 24 months. Or a 12-month waiting period for major. During the dental plan waiting period the dental insurance company will not pay for certain procedures.
On the other hand your dental plan may have a 6- or 12-month waiting period for certain services. Waiting periods typically last anywhere from 6 to 12 months and the length of the waiting period is often dependent on the type of procedure at stake. That means you have to be enrolled in the plan for at least 12 months before the.
So after your plans effective date your benefits will normally cover preventive dental care. Waiting periods are the period of time when your dental plan will not cover a specific service or benefits. Basic procedures typically include fillings or non-surgical extractions.
Cardiovascular care and cancer - Up to 2 years. Waiting out a waiting period. Fortunately it is possible to find dental insurance with no waiting period.
Dental care - 6 to 12 months. Waiting periods protect members who make payments to a fund over time for when they might need to use their health cover. If you need a family.
You can expect to pay about 30 to 45 a month for individual coverage. Some basic procedures may have a three- to six-month waiting period. However the 12 month pre-existing condition waiting period does not apply to hospital or hospital substitute treatment for psychiatric treatment rehabilitation treatment or palliative care.
This is necessary to keep health cover fair. Optical bonus Ultra bonus. A waiting period is the amount of time usually in months that a person must wait before that service or treatment will be covered by the insurance policy.
Some plans might feature one flat waiting period before any benefits begin. Dental insurance waiting periods help keep. Updated March 08 2021 A dental insurance waiting period is the length of time after purchasing your dental benefits plan that you must wait before you can use your full coverage.
Intraoral films extraoral films and panoramic films. If we didnt have waiting periods people could join a fund to claim for a. Waiting periods for major dental procedures rely on a variety of factors and can vary between health funds policies and the type of procedure.
Major work may have a three-month to one-year waiting period. Waiting periods range from 6 to 12 months. A 12-month waiting period applies for orthodontic treatment.
Some dental policies include a 12 month waiting period for major procedures. Unfortunately many dental insurance plans require a waiting period for certain services meaning treatments like fillings and root canals wont be covered for six months to a year or longer after. Major work generally include crowns bridges and dentures.