Medicare will only cover Hepatitis C screening tests if your primary care doctor or other primary care provider orders them. Medicaid FFS programs in nine states only cover hepatitis C treatment provided by specialists such as hepatologists.
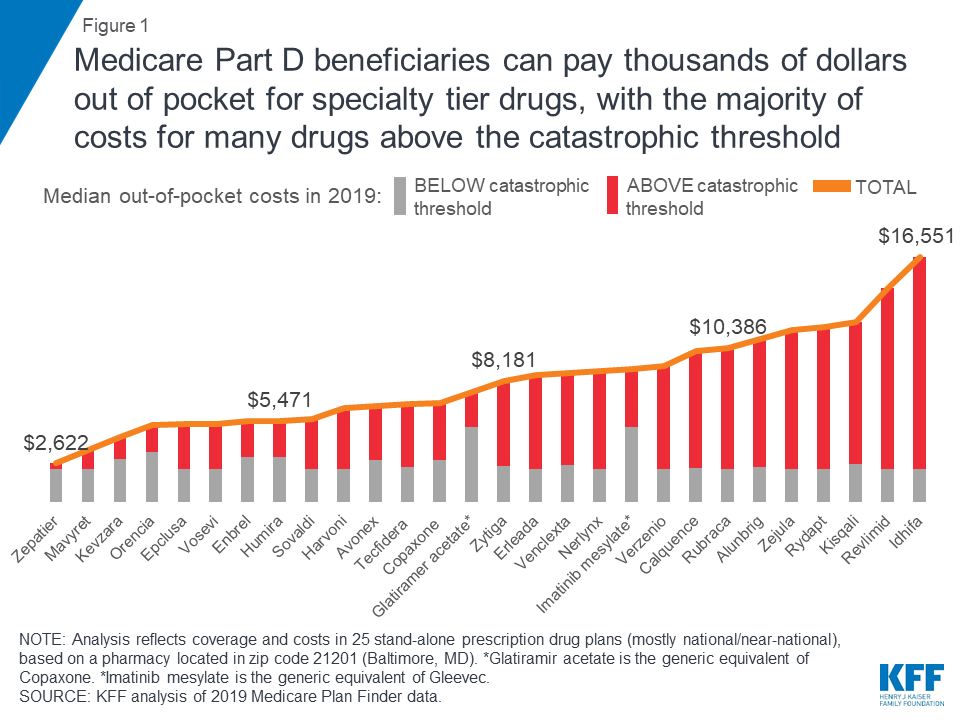 The Out Of Pocket Cost Burden For Specialty Drugs In Medicare Part D In 2019 Kff
The Out Of Pocket Cost Burden For Specialty Drugs In Medicare Part D In 2019 Kff
This doesnt mean the medications have a low cost however.

Will medicare part d pay for hep c treatment. Part D covers the herpes zoster vaccine as a preventive service. Ryan Clary of the National Viral Hepatitis Roundtable a patient advocacy group says Medicares new stance on paying for new hepatitis C treatments will. Therefore you may pay more for your drug.
But its almost certain that potent new drugs for hep-C could cure him. Coverage for hepatitis C drugs in Medicare Part D. In each scenario we assume a 12-week course of treatment of Sovaldi by itself at a total price of 84000.
Different Medicare Advantage plans have different criteria for the coverage of vaccines. KEY TAKEAWAYS Medicare Part D plans cover all commercially available vaccines except those Medicare Part B. However the private insurer that handles his medication coverage for the federal Medicare program has twice refused to pay.
Under the current Part D benefits HCV drug users with no subsidy face sizable financial burdens even with catastrophic coverage and the recent in-gap discount for brand name drugs. If your doctor has suggested naltrexone as part of a treatment plan you may have questions especially if you have hepatitis C. For four hepatitis C drugs in our analysis Epclusa Vosevi Sovaldi and Harvoni Part D enrollees can expect to pay more than half of their total out-of-pocket costs in the catastrophic phase.
Not valid for patients enrolled in government health care prescription drug programs such as Medicare Part D and Medicaid. Even if you do not fall into the risk categories for hepatitis A Medicare Part D would cover hepatitis A vaccine. Patients in the coverage gap known as the donut hole also are not eligible Harvoni at no charge for eligible and qualified uninsured patients.
In addition 28 require that. The federal Medicare program for the elderly and disabled will cover two new drugs that can cure hepatitis C a liver disease that can cause cancer and lead to death. In the Donut Hole also called the Coverage Gap stage there is a temporary limit to what Medicare will cover for your drug.
In the first scenario we assume that 25000 Medicare beneficiaries or roughly 10. But its almost certain that potent new drugs for hep-C could cure him. However the private insurer that handles his medication coverage for the federal Medicare.
The recent arrival of new hepatitis C virus HCV drugs has brought fiscal pressures onto Medicare Part D. In the Post-Donut Hole also called Catastrophic Coverage stage Medicare should cover most of. After your deductible has been satisfied you will enter the Post-Deductible also called Initial Coverage stage where you pay your copay and your plan covers the rest of the drug cost.
READ MORE A Full List of Hepatitis C Medications. As of July 2015 Medicare requires all Part D formularies to cover at least one medication that treats hepatitis C. Since people who are enrolled in Medicare are enrolled for the rest of their lives treatment for HCV now avoids the even-higher costs for the program in treating liver injury cancer or possibly.
Most eligible patients will pay no more than 5 per co-pay restrictions apply. Spending on HCV drugs in Part D jumped from 283 million in 2013 to 45. Does Medicare Part D cover the shingles herpes zoster vaccine.
The doctor recommending it must accept Medicare assignments to receive the coverage benefits. See the model scenarios in this fact sheet to decide whether to bill the patient or the Part D plan. Alternately you can also sign up for a Medicare Advantage plan to receive coverage for vaccines.