Use this tool to help calculate someones income. This means you have.
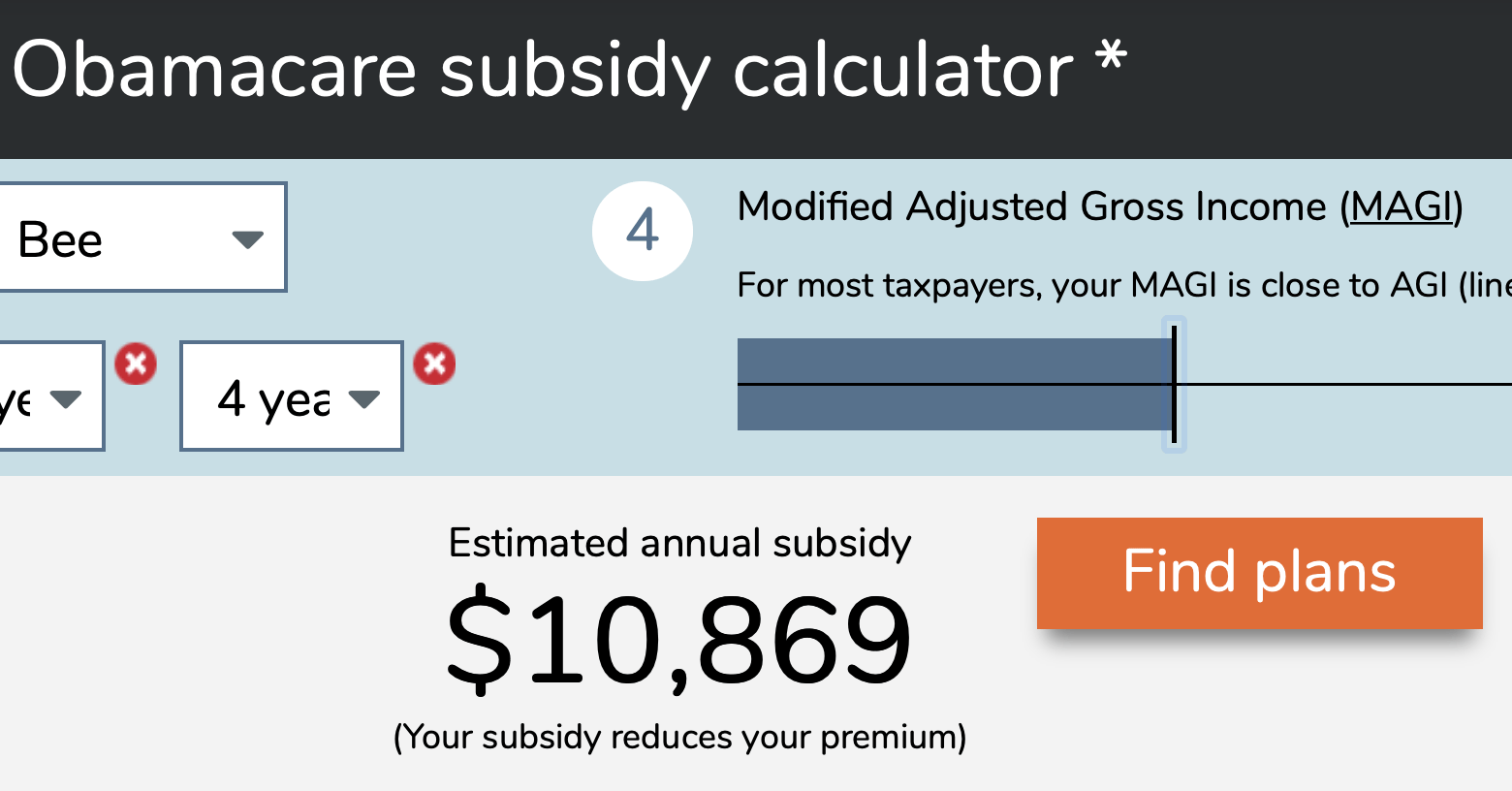 2021 Obamacare Subsidy Calculator Healthinsurance Org
2021 Obamacare Subsidy Calculator Healthinsurance Org
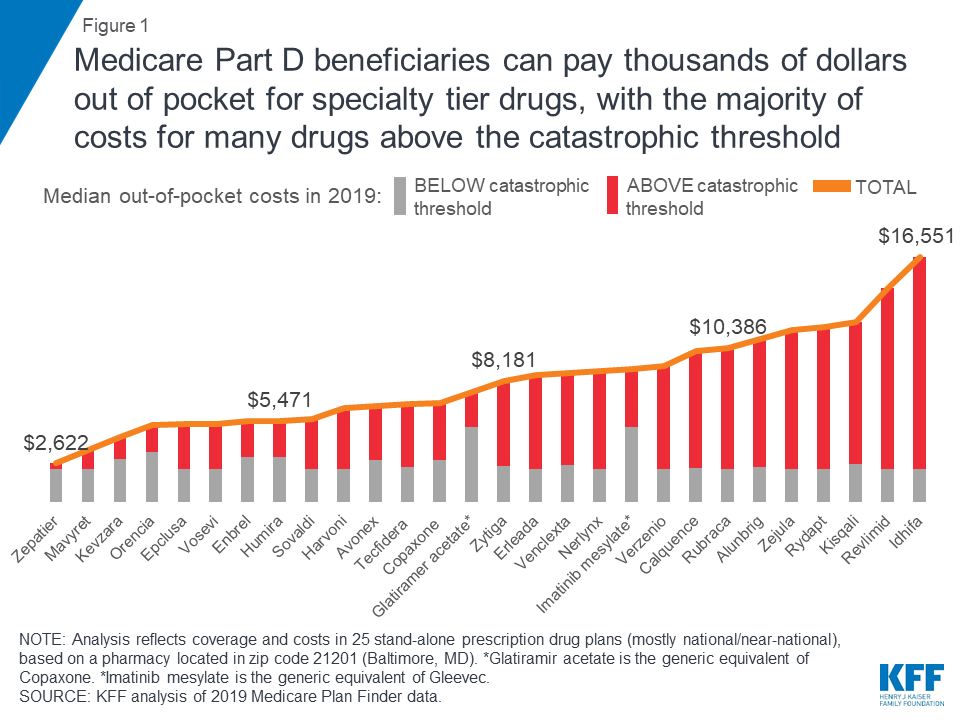
The average subsidy amount in 2020 was 492month which covered the large majority of the average 576month premium note that both of these amounts are lower than they were in 2019.
Health insurance marketplace calculator 2020. The premium tax credit is limited by comparing the cost of your coverage to that of the second. The financial help you can get to lower your monthly payment is called a Premium Tax Credit. A silver plan is a health insurance plan where the insurer pays on average 70 of the cost of covered services.
Individual health insurance mandate in 2020 and you didnt have qualifying coverage or an exemption youll be charged a fee when you file your 2020 state taxes but not your federal taxes. Health Insurance Marketplace Step One. See health coverage choices ways to save today how law affects you.
Our calculation is based upon the federal poverty level data provided by the government. Oregon Health Plan OHP Application questions. The purpose of this subsidy calculator is to provide Americans with the ability to quickly determine if they are eligible for subsidized health insurance under the Affordable Care Act.
Here are important dates to remember and some things you can do to get ready. Apply for Health Insurance Today Get Started Here. This health insurance cost calculator illustrates health insurance premiums and subsidies for people purchasing insurance on their own in new health insurance exchanges or Marketplaces created by the Affordable Care Act ACA.
Additionally this website is not associated with sanctioned by or managed by the federal government. Or just use one of the ObamaCare subsidy calculators found below for a quick estimate on marketplace cost assistance. Marketplace insurance plans are categorized by metal levels.
By submitting your information and clicking Finish you expressly consent to receiving phone calls e-mails. The metal level is based on how much the insurer pays for services covered under the plan. Beginning in October 2013 middle-income people under age 65 who are not eligible for coverage through their employer Medicaid or Medicare can apply for tax.
Enter the required information into the fields below then calculate your results. Estimating your expected household income for 2021. The 2020 Open Enrollment Period runs November 1December 15 2019.
Enroll now for 2021 coverage. Use this quick health insurance tax credit guide to help you understand the process. 800-699-9075 toll-free Coverage questions.
Official site of Affordable Care Act. Health Insurance Marketplace 2020 learn all the necessary information before enrolling in health coverage through Marketplace Exchange. This subsidy calculator is provided by My1HR a licensed Web Based Entity WBE which is certified by the Centers for Medicare and Medicaid Services CMS to connect consumers directly with the federal health insurance Exchange at HealthCaregov.
Compare 2020 health insurance marketplace rates. About the 2020 2021 Obamacare Subsidy Calculator. Our ObamaCare calculator will help you calculate tax credits and subsidies for health insurance sold on the Health Insurance Marketplace.
Less than one month til 2020 Marketplace Open Enrollment. Connect for Health Colorado is the only place you can apply for financial help to lower the cost of private health insurance. Check with your states tax department or your tax preparer to find out if theres a fee for not having health coverage.
You have less than one month until you can enroll in a 2020 Marketplace health insurance plan. Bronze silver gold and platinum. Read articles on finding the most affordable and best health insurance for yourself and family while getting ahold of the changes to the current healthcare.
You may owe the. Select your income range. This website is privately owned and all information and advertisements are independent and are not associated with any state exchange or the federal marketplace.
Enroll in an on-exchange Obamacare plan online or an off-exchange plan. 800-273-0557 toll-free Oregon Health Insurance Marketplace. Again subsidies have increased for 2021 and will remain larger in 2022 due to the American Rescue Plan.
Savings are based on your income estimate for the year you want coverage not last years Use our income calculator to make your best estimate. Get help completing the application process from Connect for Health Colorados state-wide network of certified. 2018 Subsidy Calculator Health Insurance Marketplace.
855-268-3767 toll-free infomarketplaceoregongov Contact us Follow us on social media. I didnt have health coverage in 2018 or an earlier year. Call For Health Quotes.
Key dates deadlines. You can probably start with your households adjusted gross income and update it for expected changes. Explore all 2020 options and save.