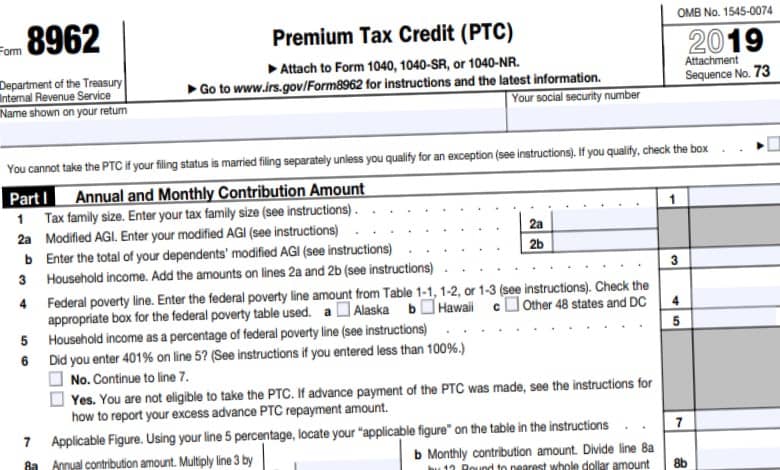
7 day supply limit for opioid naïve patients. In 2021 the initial deductible for Medicare Part D will increase slightly.
 Medicare Prescription Drug Coverage What Do I Need To Know Aetna Medicare
Medicare Prescription Drug Coverage What Do I Need To Know Aetna Medicare
Getting a 90-day supply right at your front door is better than the 30-day supply you obtain after the doctor.

Medicare part d 90 day supply. The VA operates local pharmacies all over the country. A hard safety edit stops the pharmacy from processing a prescription until an override is entered or authorized by the plan. A transition refill also known as a transition fill is typically a one-time 30-day supply of a drug that you were taking.
The comprehensive program provides extensive drug coverage and. Some plans make 90-day supplies available through some retail pharmacies in their networks as well as through mail order. Mason takes the lower-cost drug but has side effects or limited improvement Dr.
For most people the lower-cost drug works as well as the higher-cost drug. If your medication is still a part of the Medicare program you can ask your Medicare prescription drug plan for a one-time 30-day transition fill or temporary supply of your medication. If you have a Medicare drug plan and your state has issued a warning of a possible emergency or disaster.
Expand Part D vaccine coverage. During the COVID-19 pandemic Medicare drug plans must relax their refill-too-soon policy. Part D plans are expected to implement a hard safety edit to limit initial dispensing to a supply of 7 days or less.
If your doctor writes you a prescription for a higher quantity than your Medicare Part D. The AARP MedicareRx Preferred plan we sampled in New York comes with a 0 deductible but it may have a higher premium than other United Healthcare prescription drug plans. Those with current prescriptions may order refills by mail phone or online.
Veterans Affairs is one of the originators of the mail-order pharmacy business. SilverScript Choice Medicare Part D Drug Plans. Sometimes a particular medication is excluded from the Medicare Part D program and will not be available through your Medicare Part D plan - or a drug is subject to additional.
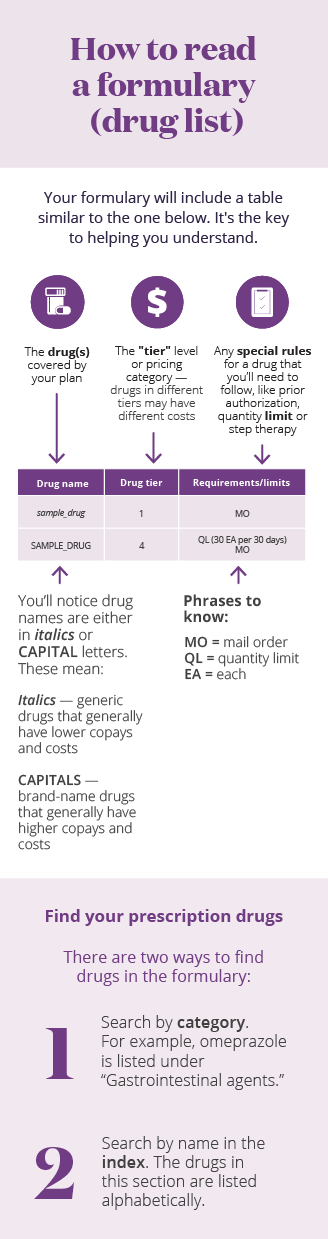
While most Part D plans allowed 90-day refills for generic drugs prior to the pandemic and half did for branded drugs the vast majority of Part D enrollees were in plans where they could not. Mason to use a lower-cost ACE inhibitor first. 75 percent coverage for generics and brand names when youre in the Medicare Part D coverage gap or donut hole.
SilverScript is a Part D prescription drug program. Low copayments for 90-day-supply mail-order prescriptions. The standout feature of this plan is that using the preferred mail order pharmacy secures 0 Tier 1 and Tier 2 copayments for a 90-day supply.
Can I get my drugs both at a local pharmacy and by mail order under the same Part D. For example in our Drug Finder or Formulary Browser we will show Q628Days next to a certain drug - meaning the quantity limit for the drug is 6 pills per 28 days - or if you see Q90365Days this means that the Medicare Part D plan limits this drug to 90 pills for the entire year. The initial deductible will increase from 435 in 2020 to 445 in 2021.
The plan rules require Mr. Step 2 If Mr. The idea isnt new.
Before switching to a different Part D plan either stand-alone or through a Medicare Advantage Plan Or before your current plan changed its coverage at the start of a new calendar year. Plans must let you get up to a 90-day supply in one fill unless quantities are more limited for safety reasons. Smith can prescribe the higher-cost ACE inhibitor.
Can I get a 90-day supply of my drugs. You may get a 91-98 transition supply or 31 day supply per fill or greater if packaging cannot be reduced to a 31 day supply or less. In light of the coronavirus pandemic the Coronavirus Aid Relief and Economic Security CARES Act requires Medicare Part D plans to provide up to a 90-day 3 month supply of covered Part D.
Contact your plan to find out. Once you spend 445 in 2021 your drug plan will pay its share of the cost of covered prescriptions. Pay a 0 copay for Tier 2 drugs and save on Tier 3 drugs on a 90-day supply at preferred retail.
From other prescription drug coverage will have obtained extended eg 90-day supplies of maintenance drugs prior to the last effective date of their previous coverage plans must provide a temporary 30-day fill unless the enrollee presents with a prescription. The initial deductible is the amount paid out of pocket before Medicare Part D covers costs. For 30-day supply at preferred pharmacies in the initial coverage stage.
Any time during the first 90 days of coverage and depending on how many days of medication are filled each time. Free standard mail delivery or pickup at a preferred retail pharmacy.