With the new health care reform laws will COBRA insurance still be retroactive and how does this works. The short answer is yes.
 Cobra Insurance Everything You Need To Know
Cobra Insurance Everything You Need To Know
Your COBRA coverage will then be retroactive to the date your insurance had ended.
Can cobra insurance be retroactive. Coverage under subsidized COBRA is not retroactive. You do not want a new illness or. You will be liable for every penny.
COBRA is always retroactive to the day after your previous coverage ends and youll need to pay your premiums for that period too. Maybe the reason you are notified so late is the 60 day rule applies when the provider tries to raise the rates. Yes COBRA Benefits Are Retroactive With No Lapse In Coverage.
This means that if you incur medical bills during your election period you can retroactively and legally elect COBRA and have those bills covered. I just asked my wife who sells insurance but does not administer cobra and she says all of that is in bounds of the law to the best of her knowledge. You could probably google around and find a sample QE notice to.
You can elect COBRA and then you have 60 days to make the payment which you would do if you had a claim that needed to be paid. However your spouse and dependents in some cases can stay covered for up to three years. My wifes obgyn provider billed.
I have written before about the ability to get retroactive COBRA benefits so I knew that we would be okay. We just got an epi pen for allergies and the billed amount without insurance was 1000. John says November 14 2014 at 750 pm.
If you are going to use this do-over be very careful with your dates. This often means the individual is responsible for paying 2-3 months worth of premiums to obtain coverage. I believe the advice of getting of retroactive coverage by selecting COBRA before the end of 60 is correct.
One advantage of enrolling right away is that you can keep seeing doctors and filling prescriptions without a break in coverage. However if you expect your gap in coverage to be under 60 days then you can use the retroactive clause under COBRA to try and avoid paying for COBRA during that time. If you enroll in COBRA before the 60 days are up your coverage is then retroactive as long as you pay the retroactive premiums.
In addition dependents can elect COBRA if they lose eligibility for coverage because of. And if there is any way you can pay the insurance-negotiated price instead of the retail price. For example if employer-provided coverage ends on 630 COBRA picks up on 71.
The Federal COBRA Health Insurance Act requires all businesses with 20 or more employees to offer a continuation of the health insurance after job loss. Retroactive Nature of COBRA coverage When an individual decides to enroll in COBRA they are responsible for the full premium as of the date of the qualifying event not the date of enrollment in COBRA. The plan may continue coverage during the electioninitial payment period beyond the date that coverage would otherwise be lost due to the qualifying event and then retroactively.
COBRA coverage is retroactive if elected and paid for by the qualified beneficiary. When you elect COBRA continuation coverage the effective date begins the date after your employer sponsored health benefits had ended. However I would check with professionals to make sure that new illnesses or accidents occurring during the 60 day period will be covered under the new not COBRA based coverage.
If you were insured through COBRA before April 1 medical and premium costs incurred before then. You can wait 60 days to elect for coverage and then you actually have another 45 days to make the payment to cover the period from the date of election to the date of lost coverage. Dont make the payment.
Your previous workplaces plan administrator should give you a COBRA election form within 45 days from your job ending. So while it seems retroactive. You then have have 60 days to elect coverage or waive your right to it.
COBRA lets you keep your former employers coverage for up to 18 months. However agency guidance makes clear that health coverage may be canceled retroactively only to the extent permitted under COBRAs rulesincluding the rule extending the deadline for notifying the plan of certain events during the COVID-19 emergency. That could be a lot of uncovered bills.
Luckily for you youve had full creditable coverage so as long as you have not been without coverage for 63 days you will be perfectly fine retroactively signing up for COBRA should there be any issues in the few weeks you are between jobs. Death of the covered employee. If the employee enrolls during the 60-day period then theres no lapse in coverage because COBRA applies retroactively to the date that the employee loses coverage.
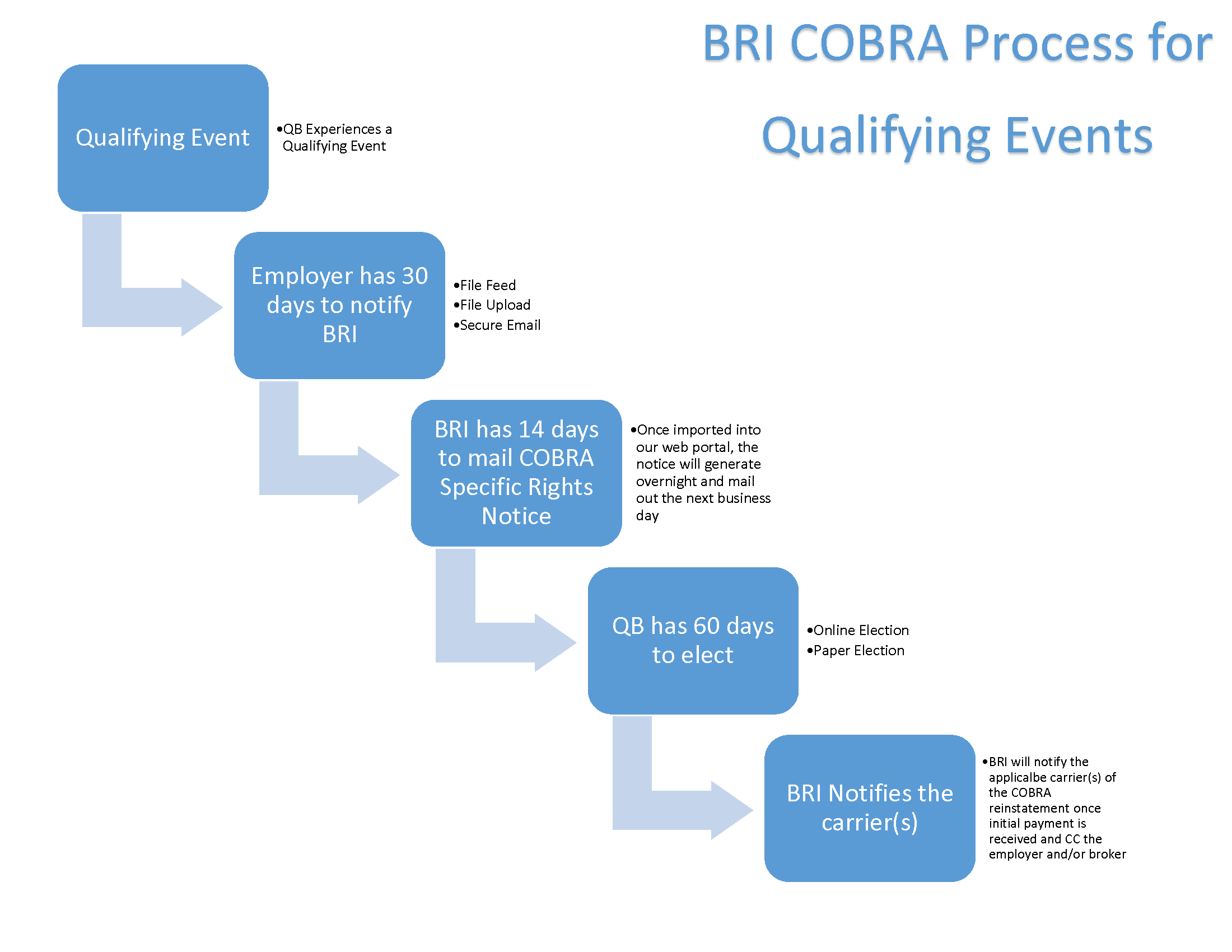
When you get your COBRA Qualifying Event notice it will give you the time frames when you need to elect and when you need to pay. Where do I send my COBRA payments. Between the provider negotiating with the government the employer and other regulation that 60 days can go by fast.
The COBRA election notice should contain the address to which premium payments should be sent and should be provided by the employer or group health plan administrator along with the amount of the premium due and its due date. Termination of benefits can be retroactive by weeks or months. This may not be a problem with the advent of ACA but I am not sure.
Your former employers insurance.