AdventHealth Group Plans fully insured. Below are printable PHC Provider Directories.
Welcome to The Empire Plans Online Participating Provider Directory.
Medical plan provider directory. This directory is for. Colorado Tier 1 Providers. Molina Healthcare of California Partner Plan Inc.
For employees of AdventHealth. We include the most current lists of in-network providers and facilities in our online provider directories. Some network providers may have been.
We have an extensive list of participating providers hospitals and pharmacies. AH Lab and Radiology Tier 1 Providers. To help you find the right in-network provider in your plan log in to your myPRES account.
This directory is current as of October 1 2016. Sometimes CCP does not receive a. Any inaccurate information may be reported by calling 1-888-936- PLAN 7526 or emailing us at providernetwork.
This Provider Directory is your first step towards better health. For the most current information please use the searchable directory. There is a nationwide.
CCP checks this information at least every 3 years. For members in out-of-state locations select a link below to view Tier 1 in-Network providers. Miami-Dade Broward and Palm Beach counties.
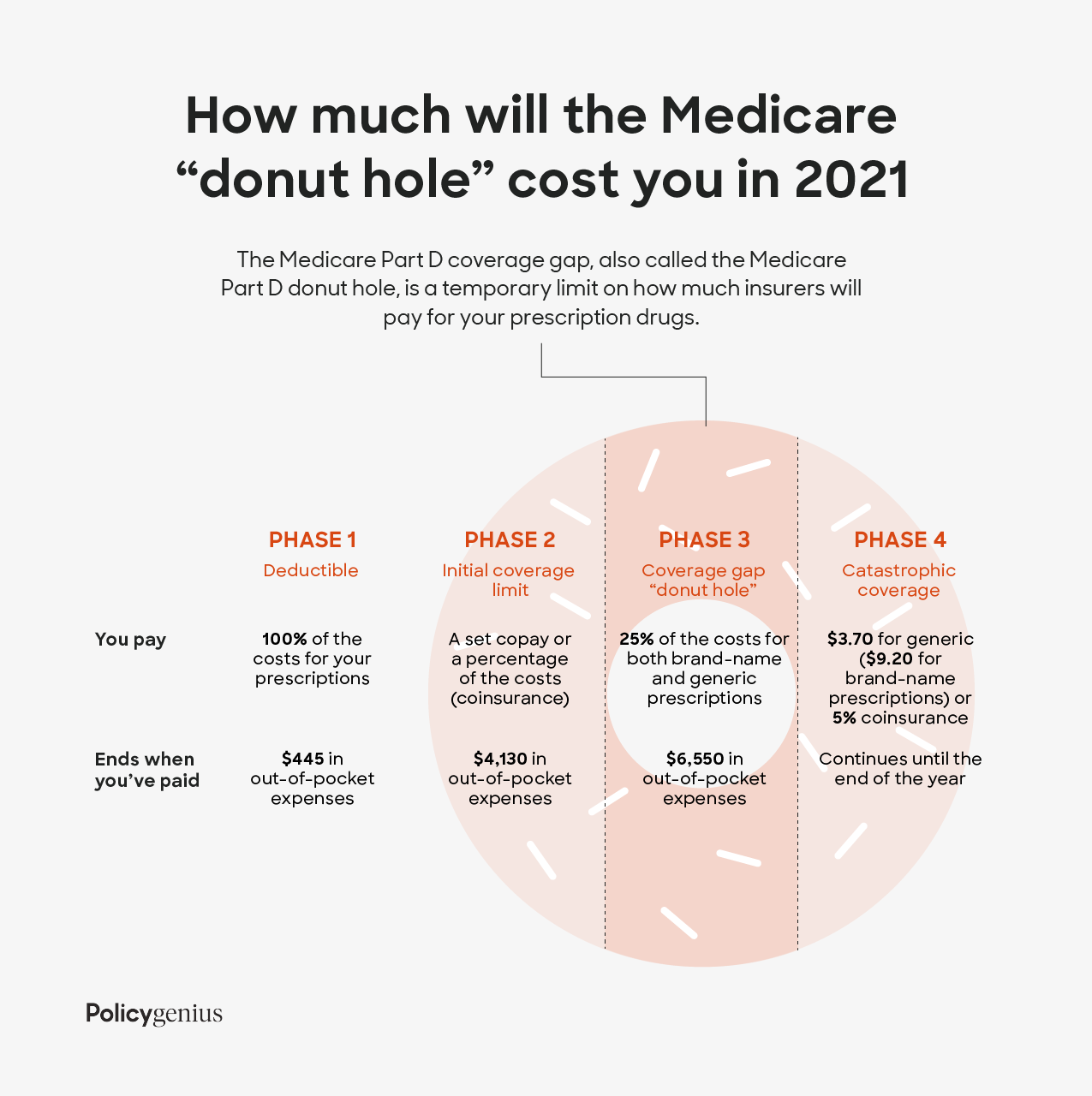
This means that you will pay the same cost sharing amount for your prescriptions in all 50 states and the District of Columbia at any of our in-network pharmacies. Health Care Provider Directory. It lists all of the doctors clinics and other providers that accept Health Plan members.
711 Specialty Health Plan Family Health Centers of San Diego 619 515-2445. UnitedHealthcare Community Plan 866 270-5785TTY. Providers and regions may vary by plan.
The doctor or hospital gives CCP this information on their application when they join the health plan. Joseph Sugarland Willowbrook and the Methodist Hospital networks as well as Southeast Texas and Southwest Louisiana. The Secure HMO plan does not include coverage for Part.
With The Empire Plan you can choose a participating provider or non-participating provider for medical services. Here you can search for providers that participate with Contra Costa Health Plans two networks consisting of over 5000 primary care providers and specialists. 888 665-4621 TTYTDD 800 479-3310.
Download the latest digital version of the Provider Directory here. This directory is current as of August 20 2020. AdventHealth System Employee Health Plan.
This directory is for covered CHRISTUS Health Plan USFHP members in the Houston and Surrounding Areas. AdventHealth Medicare Advantage Plans. Search for Tier 1 providers Select AdventHealth Employee Health Plan from the Network menu.
Make your selection All Provider Types Birth Centers Boarding and Lodging Providing Special Services Boarding Care Homes Community Mental Health Center Medicare Comprehensive Outpatient Rehab. To 800 PM seven days a week from October 1 through March 31 and 800 AM. Health First Brevard County FL Health Insurance Plans Space Coast Healthcare Provider Hospital Services.
North Carolina Tier 1 Providers. Medi-Cal Provider Directory Los Angeles County Molina Healthcare JSON Medi-Cal Provider Directory Sacramento County JSON Medi-Cal Provider Directory San Diego County JSON Medi-Cal Provider Directory San Joaquin County JSON Medi-Cal Provider Directory Stanislaus County JSON Medi-Cal Provider Directory Tulare JSON. Rosen Hotels and Resorts Health Care Plans.
This directory gives members potential members and providers access to our network of physicians pharmacies hospitals and ancillary providers. Step 1 Select a provider type. Below we describe the information in the fields in the provider directory.
2021 Provider Directory. Find care with UPMC Health Plans Provider Directory. Kansas Tier 1 Providers.
Printed directories are updated every 30 calendar days. Use our online directories to search for doctors specialists or hospitals that accept The Health Plan insurance. You may print selections directly from the searchable directory or you may request a copy of a Provider Directory by contacting our Member Services Team at 800 863-4155.
3 Steps to locating Minnesotas licensed registered or certified health care providers. Monday to Friday from April 1 through September 30. You may request a hard-copy of Provider Partners Health Plans Provider Directory by calling Member Services at 800-405-9681 TTY users call 711 800 AM.
We offer national in-network prescription drug coverage. Your health plan materials are the best source to help you understand your covered services and providers. Information on provider qualifications specialties and board certifications are included in our online directories.
You can register for access to our secure provider portal where you can conduct many transactions such as Verification of member eligibility benefits Authorization requests status PCPs Only View Hospital Admission Discharge PCPs Only Submit transactions twenty-four hours a day seven days a week Increased accuracy of data and avoid duplication Submission of claims view claims status and. AdventHealth Advantage Plans is proud to offer a quality network of more than 4000 physicians and the areas premier hospitals. Browse doctors by specialty procedure service or equipment to find the best fit for you.
Health First Health Plans is proud to offer a quality network with more than 4000 physicians and the areas premier hospitals. Additional information on medical school attendance or residency completion is available by calling our Customer Service Department. You will need to submit claim forms and pay a higher share of the cost if you choose a non-participating provider or non-network provider.
This directory provides a list of Solis Health Planscurrent network providers.








/GettyImages-1126401283-f3f8d3d9ba45453ba87d052322307519.jpg)