What is Your Plan Paying For. PBMs have two main objectives.
Pharmacy Benefit Management Industry Definition
These can include drugs that must be given to you by a health care provider.

Pharmacy benefit plan. You may also view a general PDL but youll need to confirm your specific coverage details before filling a prescription. And to help patients achieve better health outcomes through greater access to appropriate medications. How to find and use your Prescription Drug List PDL You can sign in to your health plan account and look under your pharmacy and prescription coverage information to see your plans PDL.
Our two- and three-tier plans give you both generic and brand name prescription drug coverage. Some plans require use of an in-network pharmacy or designated home delivery pharmacy for coverage to apply. Support for some complex health conditions.
Being an Aetna prescription drug plan member has its perks. They do this through affecting the behaviors of pharmacists and doctors to prescribe drugs appropriately to maximize their effectiveness. A pharmacy benefit manager also known as a PBM is an organization that provides services educational programs and services to aid patients.
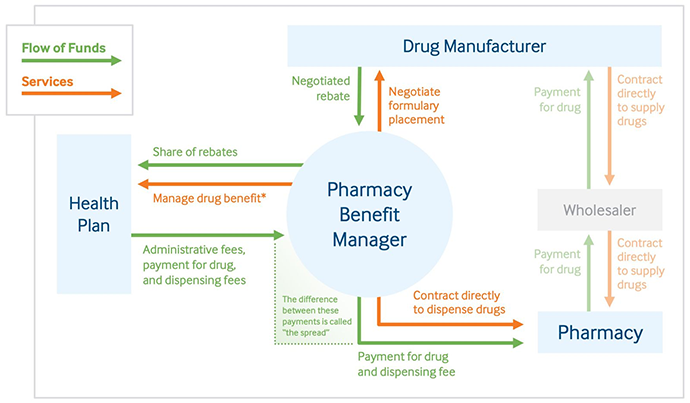
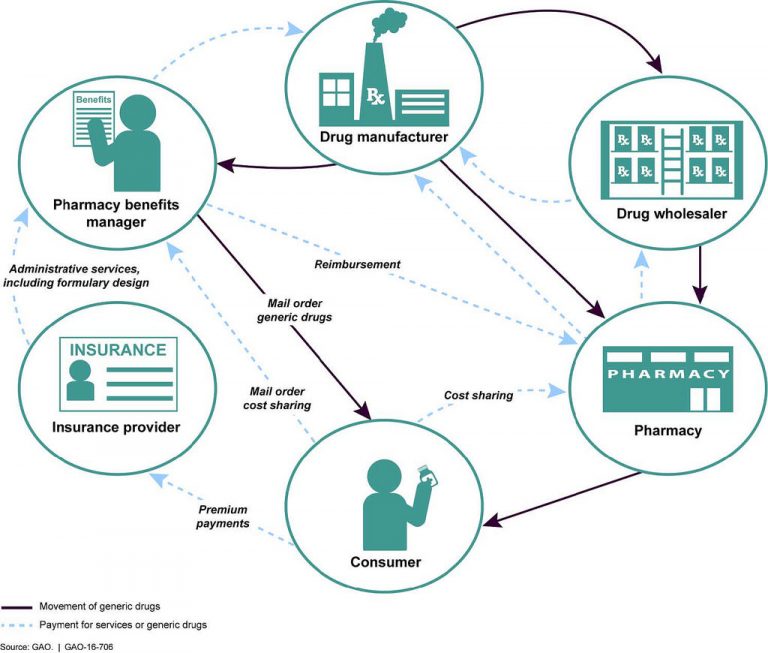
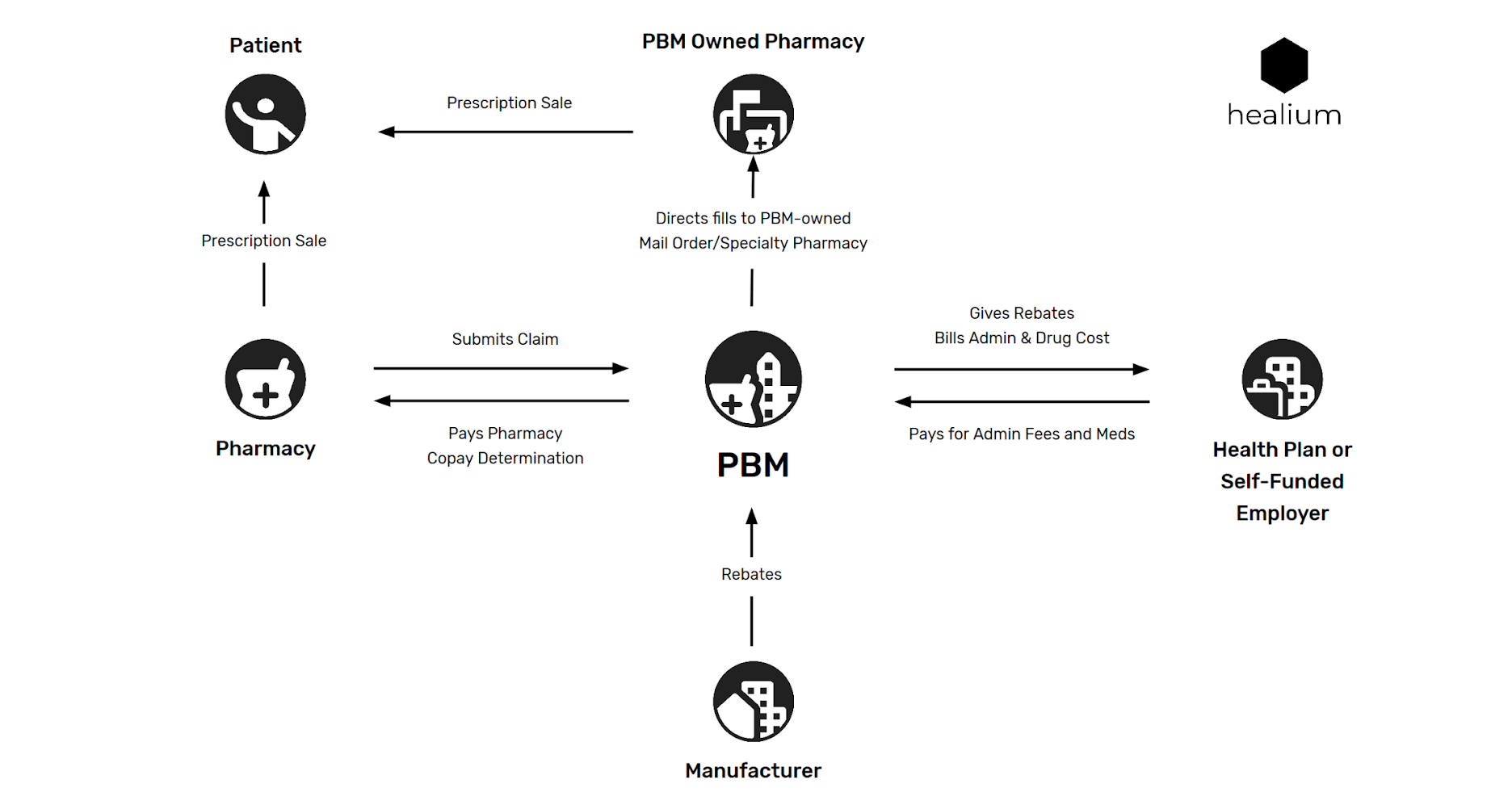
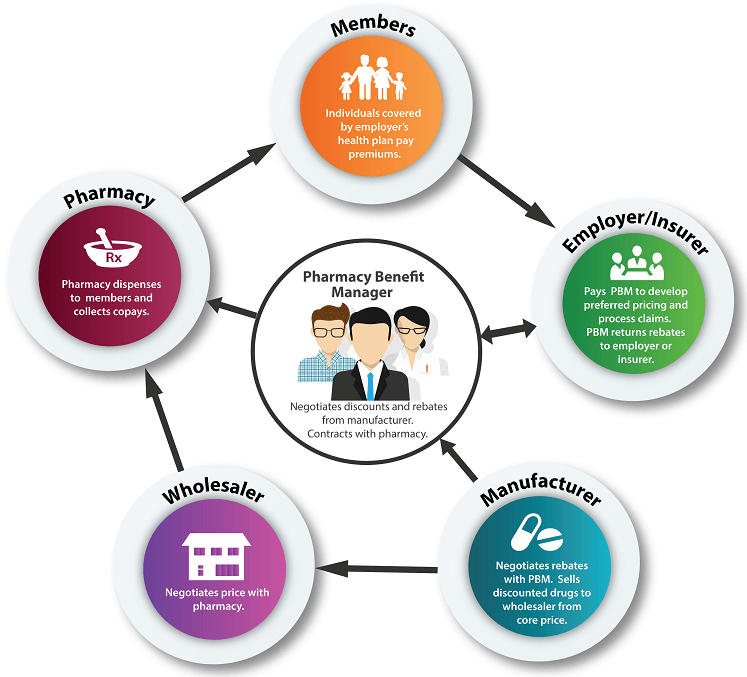
Pharmacy benefits and services Get extra support with your pharmacy coverage. These drugs are often given to you in a hospital doctors office or health care setting. A PBM also negotiates discounts and rebates with drug manufacturers.
1 Health benefit plans vary but in general to be eligible for coverage a drug must be approved by the Food and Drug Administration FDA prescribed by a health care professional purchased from a licensed pharmacy and medically necessary. Treatment for certain chronic conditions often means taking a. In contrast to a carve-in strategy carve-out plans give employers better control over pharmacy benefit costs a crucial consideration as the costs of prescription drugs continue to rise.
Pharmacy Benefit Management Elixir provides unconventional levels of service clarity and control. It contracts with pharmacies and builds and maintains drug formularies. Some plans may also have a Specialty Tier which is covered under the pharmacy benefit.
Coverage may be subject to plan deductible copayment andor coinsurance requirements. April 07 2021 The world of pharmacy benefits continues to get more complicated and that is unfortunately not an accident. Health plans may administer medical and pharmacy coverage separately for select drugs.
Some drugs are covered under your medical plan instead of your pharmacy benefits. To curate pharmacy prescription benefits plan options. Lauren Vela of the Pacific Business Group on Health examines how large self-insured employers and other health plan sponsors can remove low-value or wasteful drugs from their pharmacy benefit plans and save 3 percent to 24 percent of outpatient pharmacy costs managed by pharmacy benefit managers.
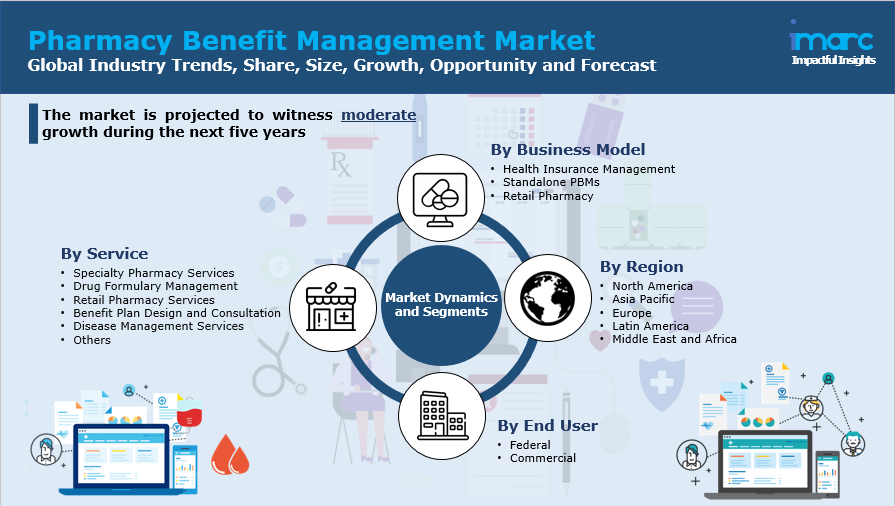
Today the specialty pharmacy market is approximately an 87 billion industry with most specialty pharmacy providers owned by PBMs health plans or pharmacy. Amongst a healthcare industry where consolidation is prevalent it can be hard to find a partner with the adaptability to meet your needs. Pharmacy benefit managers also known as PBMs such as Optum CVS Health and Express Scripts cover more than 80 of the American publics pharmacy needs.
Comprehensive pharmacy services would mean having the pharmacy team develop the management strategy for specialty medications used under either the medical benefit or the pharmacy benefit. This content requires JavaScript. A pharmacy benefit manager PBM processes and pays prescription drug claims for its members.
Fee Schedules and Appendices describes the structure of the pharmacy benefit plan for claimants in New Yorks Workers Compensation system. Carve-out plans give employers transparency into their pharmacy benefits allowing them to have greater understanding and control of spending negotiate better deals and ensure the. Members who have home delivery coverage only will not be able to utilize Pharmacy Locator.
The current pharmacy benefit plan which has been in effect since July 11 2007 defines the payment. This service is available only to Plan Members who have a retail drug program administered by Express Scripts. All group health insurance policies and health benefit.
To do this PBMs work with drug manufacturers wholesalers pharmacies and plan sponsors. Part 440 describes the Pharmacy Fee Schedule applicability etc. Through the pharmacy benefit manager PBM or pharmacy benefit optimizer PBO your clients can access valuable programs and tools that provide protection against unnecessary plan spending on high-cost drugs.
Pharmacy Benefit Managers. You get easy-to-use pharmacy programs that offer the convenience you want with the value youre looking for.
What Is A Pbm Enabling Healthy Decisions
 Role Of Pharmacy Benefit Managers In The Pharmaceutical Supply Chain
Role Of Pharmacy Benefit Managers In The Pharmaceutical Supply Chain
 Pharmacy Benefit Management Market Share Size Growth Opportunity And Forecast 2021 2026
Pharmacy Benefit Management Market Share Size Growth Opportunity And Forecast 2021 2026
 Drug Channels Follow The Dollar Math How Much Do Pharmacies Wholesalers And Pbms Make From A Prescription
Drug Channels Follow The Dollar Math How Much Do Pharmacies Wholesalers And Pbms Make From A Prescription
:max_bytes(150000):strip_icc()/largest-pharmacy-benefit-managers-2663840-FINAL-5be9a0b746e0fb0026ca5bd6.png) How Pharmacy Benefit Managers Pbms Work
How Pharmacy Benefit Managers Pbms Work
 Pbm Industry To Consolidate Power
Pbm Industry To Consolidate Power
Https Le Utah Gov Audit 19 13rpt Pdf
 Pbm Pharmacist Work From Home Pbm Pharmacist Jobs
Pbm Pharmacist Work From Home Pbm Pharmacist Jobs
 Reducing Wasteful Spending In Employers Pharmacy Benefit Plans Commonwealth Fund
Reducing Wasteful Spending In Employers Pharmacy Benefit Plans Commonwealth Fund
 The Relationship Between Pharmacy Benefit Managers Pbms And The Cost Of Therapies In The Us Pharmaceutical Market A Policy Primer For Clinicians Sciencedirect
The Relationship Between Pharmacy Benefit Managers Pbms And The Cost Of Therapies In The Us Pharmaceutical Market A Policy Primer For Clinicians Sciencedirect
 How Pharmacy Benefit Managers Pbms Work By Nick Wimpey Healium Medium
How Pharmacy Benefit Managers Pbms Work By Nick Wimpey Healium Medium
Pharmacy Benefit Management Industry Definition
 Pharmacy Benefit Manager Pbm Games Youtube
Pharmacy Benefit Manager Pbm Games Youtube
 How Employer Plans Cover Prescription Drugs Infographic Medcost
How Employer Plans Cover Prescription Drugs Infographic Medcost

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.