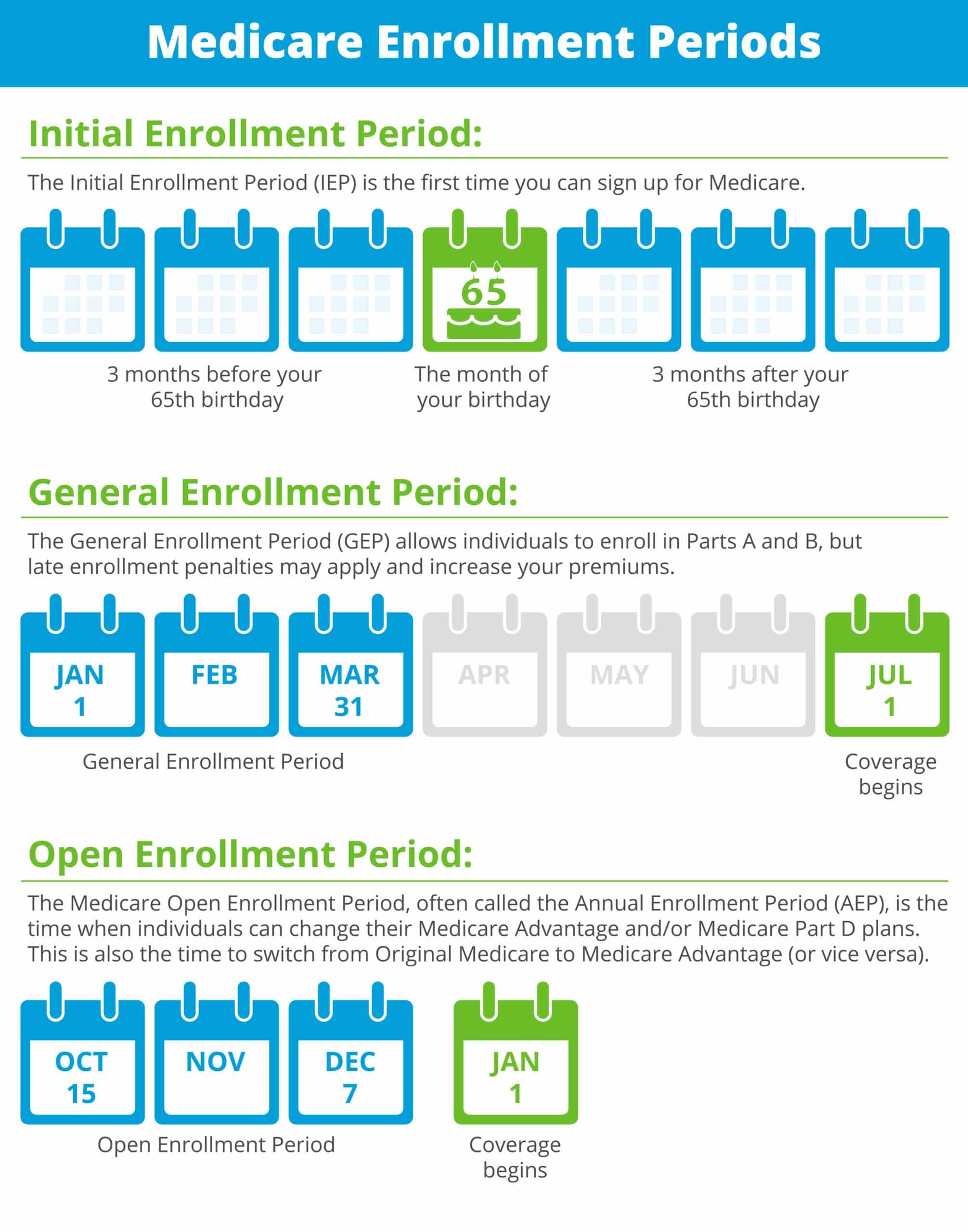
You do not need to select a primary care physician and you do not need referrals to see other providers in the network. The Availity Portal offers health care professionals free access to real-time information and instant responses in a consistent format regardless of the payer.
/Anthem-8f83a86e14b94fa5a570b5f83374df3d.jpg) Anthem Medicare Insurance Review
Anthem Medicare Insurance Review
As an Anthem PPO member regardless of your choice you will still have the same access to your UCLA doctor as you have today.

Anthem access ppo. THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN. A Medicare Advantage PPO plan is one type of Medicare Advantage plan. You do not need to select a primary care physician and you do not need referrals to see other providers in the network.
By signing your name and returning the enclosed Enhanced Care Coordination Participating Member Form you are taking the first step towards enhanced care coordination. Anthem MediBlue Access PPO is a Local PPO. We offer deep discounts and one of the largest dental networks in the nation along with ways to customize our plans for total flexibility.
Click Here to Enroll Online Click Here to Call 844-938-0419. You are the most important part of the team. Anthem MediBlue Access PPO is a Local PPO.
For more recent information or other questions please contact Anthem MediBlue Access PPO Customer Service at 1-833-344-1012 or for TTY users 711 24 hours a day 7. This summary does not reflect each and every benefit exclusion and limitation which may apply to the coverage. Total Premium Includes Part B 18950.
Anthem Gold Blue Access PPO 400005000 Plan name Network Blue Access Blue Access Blue Access Blue Access Blue Access Blue Access Blue Access Contract code 4F1N 4EYX 4EZV 4F13 4EZD 4F27 4EXM Deductible1 individualfamily 40008000 20004000 25005000 27005400 35007000 45009000 45009000 Coinsurance 0. Anthem MediBlue Access PPO is a Local PPO. A preferred provider organization PPO is a Medicare plan that has created contracts with a network of preferred providers for you to choose from at reduced rates.
You do not need to select a primary care physician and you do not need referrals to see other providers in the network. A preferred provider organization PPO is a Medicare plan that has created contracts with a network of preferred providers for you to choose from at reduced rates. If your market doesnt use Availity for secure provider tasks please return to the Provider Overview page for additional state-specific.
Find drug lists pharmacy program information and provider resources. Anthem Gold Blue Access PPO 3000207000 Anthem Gold Blue Access PPO 250007500 Plan name Network Blue Access Blue Access Blue Access Blue Access Blue Access Blue Access Blue Access Deductible1 individualfamily 25005000 30006000 15003000 22504500 25005000 25005000 40008000 Non-network deductible. If you choose to see a provider outside your plan your costs may be higher.
You do not need to select a primary care physician and you do not need referrals to see other providers in the network. A preferred provider organization PPO is a Medicare plan that has created contracts with a network of preferred providers for you to choose from at reduced rates. A preferred provider organization PPO is a Medicare plan that has created contracts with a network of preferred providers for you to choose from at reduced rates.
This formulary was updated on 4202021. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. For more details important limitations and exclusions please.
Anthem Blue Cross. Anthem MediBlue PPO is a Medicare Advantage plan that gives you the flexibility to work with any doctor or specialist in or out of network no referrals needed. Anthem MediBlue Access PPO is a Local PPO.
A preferred provider organization PPO is a Medicare plan that has created contracts with a network of preferred providers for you to choose from at reduced rates. Anthem MediBlue Access PPO is a Local PPO. Trades as Anthem Blue Cross and Blue Shield in Virginia and its service area is all of Virginia except for the City of Fairfax the Town of Vienna and the area east of State Route 123.
Log in to Availity. Anthem ChamberAdvantage Blue Access PPO 2500506000 NEW Anthem ChamberAdvantage Blue Access PPO 2500205000 Anthem ChamberAdvantage Blue Access PPO 2000207500 NEW Anthem ChamberAdvantage Blue Access PPO 2000203500 Anthem ChamberAdvantage Blue Access PPO 1500204000 Anthem ChamberAdvantage Blue Access PPO 1000203000 Anthem ChamberAdvantage Blue Access PPO. National PPO BlueCard PPO This summary of benefits is a brief outline of coverage designed to help you with the selection process.
Community Insurance Company CIC In Virginia. Anthem MediBlue Access PPO Plan Organization Type. You do not need to select a primary care physician and you do not need referrals to see other providers in the network.
For Medicare Supplement plans. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. As the nations second largest health plan-owned company Anthem Behavioral Health provides choice innovation and access.
Anthem Gold Blue Access PPO 1000207000 Plan name Network Blue Access Blue Access Blue Access Blue Access Blue Access Blue Access Pathway Group HMO Deductible1 individualfamily 10003000 15003000 20004000 25005000 30006000 15003000 5001500 Non-network deductible individualfamily 30009000. Anthem Insurance Companies Inc. Anthem MediBlue Access PPO PLEASE READ.
Anthem Health Plans of Virginia Inc. Are all Medicare Advantage Plans PPOs.






_360_255_100.jpg)